Internal Medicine Residency
Welcome to the University of Iowa Internal Medicine Residency Program
Our mission is to provide our residents with the individualized instruction and experiences that will help them excel in their future careers as clinicians, educators, and scholars.
Whether your goal is outpatient primary care, inpatient hospital medicine, fellowship, research, or if you are undecided, we’ll help you tailor your residency to be the foundation of your future personal and professional success.
We are excited about your interest in our program. We invite you to explore what Iowa has to offer.
About the Program
This website is dedicated to introducing applicants to what our residency program has to offer.
We also invite you to check out imiowa.com, which is the website the chief residents maintain. This is where our residents go to find things like the noon conference schedule (with the lunch menu), recordings of previous lectures, and other resources.
If you have any questions, please reach out to us at intmedres@uiowa.edu or 319-384-9668!
Message from the Program Director
As director of the Residency Program in the Department of Internal Medicine, it’s my honor to introduce you to the array of opportunities that exist at the University of Iowa. We believe we can provide you with the kind of individualized instruction and experiences that will help you transition from one phase of your professional career to the next. We aim to produce graduates who excel as clinicians, physician scientists, and teachers.
At our world-renowned residency, we offer:
- broad clinical experiences across both inpatient and ambulatory settings
- access to state-of-the-art facilities and equipment
- dedicated teaching faculty who are thought-leaders in their fields
- strong camaraderie with colleagues
- house-staff research opportunities
- development of teaching skills
- career counseling
We have a strong leadership team made up of outstanding associate program directors, motivated and inspired chief residents, creative and enthusiastic faculty, and dependable and involved site directors. Each of us works tirelessly to optimize the training experience for our resident physicians. Our program enables house staff to develop excellent clinical skills, while also preparing them to meet long-term career goals.
While we have a long tradition of training outstanding clinicians, we also continually work to keep our curriculum and methods cutting-edge. The program leadership works closely with chief residents and other core educators and invites input from residents in designing and refining innovative programs. For example, we’ve recently instituted a “4+1 program” that allows residents an improved ambulatory experience, guided career and mentor choice at the same time maintaining a balanced work-life experience. This allows residents to immediately begin exploring the subspecialty that interests them while also exposing them to fields they may not have previously considered.
Another example of our unique and cutting-edge program is our Master Clinician Program/Clinical Reasoning Curriculum. A pillar of our educational focus has been to teach our residents clinical reasoning and problem solving. Our residency produces life-long learners capable of unraveling the most impenetrable puzzles. No matter a resident’s area of career focus, our residency program significantly raises his or her clinical reasoning performance level.
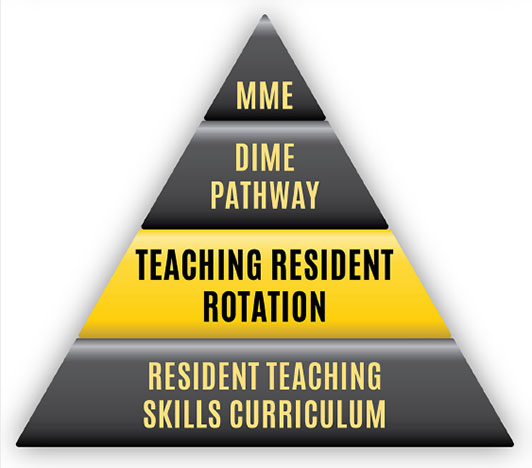
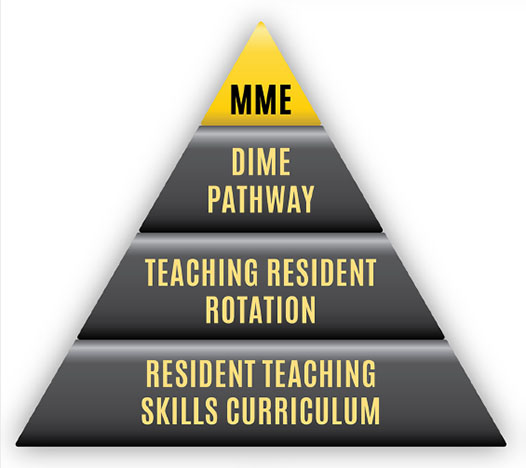
We believe that our residents should not only be life-long learners of medicine but life-long teachers of medicine. To that end, we have developed the Teaching Skills Curriculum, which many residents find complements their formal training and enhances their clinical skills. One career path a resident may consider is becoming a clinician educator and thus may be interested in pursuing a Masters in Medical Education.
We understand that every resident has unique interests and career goals, and we have developed our training program to meet as many specifications as possible. No matter the resident’s long-term career goals, our residency program taps into a wealth of knowledge and experience that exists in our department’s faculty, creating specific mentorship experiences, and offering residents career-shaping opportunities.
If you are looking for a program that will challenge you and provide you with the experience and guidance to prepare you for the next step in your career, we hope you will continue to explore the University of Iowa’s Internal Medicine Residency program. If you have any questions about any aspect or whether our program is right for you, please don’t hesitate to contact us.
Watch Dr. Suneja's 2020 Carver College of Medicine Commencement Address:
Mission and Aims
 The Department of Internal Medicine Residency Program is dedicated to educating future clinicians, physician scientists and scholars to serve the people of the state of Iowa, the nation and the world. Our program provides comprehensive, broad-based training and is dedicated to developing confident, knowledgeable, professional and caring internists who will be well prepared for their roles in the rapidly changing environment of healthcare. The three-year accredited program ensures that residents develop a strong foundation in general internal medicine so that they are able to address the wide range of problems encountered in clinical practice. The program also responds to special interests of residents by offering experiences and instruction to meet individual career goals and to help residents transition from one phase of their professional career to the next.
The Department of Internal Medicine Residency Program is dedicated to educating future clinicians, physician scientists and scholars to serve the people of the state of Iowa, the nation and the world. Our program provides comprehensive, broad-based training and is dedicated to developing confident, knowledgeable, professional and caring internists who will be well prepared for their roles in the rapidly changing environment of healthcare. The three-year accredited program ensures that residents develop a strong foundation in general internal medicine so that they are able to address the wide range of problems encountered in clinical practice. The program also responds to special interests of residents by offering experiences and instruction to meet individual career goals and to help residents transition from one phase of their professional career to the next.
Our Mission:
To provide our residents with the individualized instruction, training, and experiences that will help them excel in future careers as clinicians, educators, and scholars.
Program Aims:
- Train physicians to be lifelong learners, committed to self-reflection, self-assessment, and improvement.
- Advance clinical reasoning and judgement skills necessary to approach complex, as well as common, problems that present to the generalist.
- Empower physicians to identify social determinants of health, to address disparities and to create a system that promotes equitable access, treatment, and outcomes for all patients.
- Develop skills and knowledge in teaching, quality & safety, and scholarship.
- Provide clinical experiences allowing residents to learn, and to practice delivering, team-based care that reflects respect for patient values and preferences.
- Deliver a core curriculum allowing residents to gain knowledge that reflects understanding in the art of inquiry and science of discovery.
- Maintain a culture of wellness which prioritizes resident support, camaraderie and mentorship.
- Offer opportunities and flexibility supporting individualized career plans.
- Foster a learning environment that promotes progressive responsibility and graduated autonomy.
Core Values:
- Excellence & Integrity
- Curiosity, Discovery, Innovation
- Humanism
- Strength in Diversity
- Individualized Mentorship
- Camaraderie & Belonging
- Integrated Collaborative Learning Environment
- Scholarship
Clinical Opportunities
The development of our residents into well rounded physicians is the core of the University of Iowa Internal Medicine residency mission. This growth happens by taking care of patients in clinic and at beside.
Our program utilizes an X+Y schedule that allows for abundant patient care-experiences in both the inpatient and outpatient settings with increasing levels of autonomy as residents progress through their training. Our residents rotate for 4 weeks on an inpatient general medicine service or subspecialty consult service followed by a 1 week experience dedicated to ambulatory medicine (the Y week). This system allows for significant individualization of schedules so residents can pursue their interests in specific subspecialties or explore many different subspecialties as they decide if they want to go into a specific subspecialty or become a general internist.
If you are interested in doing a preliminary year at the University of Iowa or our medicine-psychiatry residency program, please check out the links below.
We invite you to take a tour of where you will be learning medicine by checking out our facilities.
X-Block
During the 4-week X-block, our residents rotate through core rotations that expose residents to the full breath of inpatient general medicine and a wide variety of elective rotations that provide ample flexibility for residents to tailor their experience to their career goals.
Core Inpatient Rotations
The foundation of the experience that develops our residents from medical students into independent physicians is the experience of taking care of patients on our general medicine wards. Our residents rotate on general medicine teams at the University of Iowa Hospitals and Clinics and the Iowa City VA. We offer a primary cardiology inpatient team at the University and our residents also have the opportunity to rotate on the medicine/psychiatry unit as senior residents. Our residents also get plenty of ICU experience while rotating in the Medical Intensive Care Unit and Cardiovascular Intensive Care Unit.
During the first year, our residents generally spend 6 to 7 X-blocks on a core rotation.
Our residency prioritizes the experience of one team taking care of patients from admission until discharge. Therefore, none of our core rotations have an “admitting team” and a “floor team.” Every team both admits patients and takes care of them on the floor until they discharge. We believe facilitates residents getting to know their patients personally and develop relationships with them and that is crucial to our residents growth as clinicians.
UIHC Inpatient Medicine
The University of Iowa Hospitals and Clinics (UIHC) is the only academic hospital in the state of Iowa. Consequently, many of our patients present from across the state with complicated and/or rare medical problems requiring the subspecialty care that only our institution can provide. UIHC also acts as the “safety net” hospital for the state of Iowa, providing care to the under-served populations. As such, our residents see a wide range of conditions in a diverse patient population while rotating on the general medicine floor at UIHC.
Three teams, each comprised of a staff hospitalist, one senior resident, three interns, and 2-3 medical students admit, diagnose, and manage these patients. Two interns take care of patients during the daytime and the third intern provides coverage at night every time their team is on call. On average, interns take 3-4 nights of call per X-block.
Admission are allocated based on a rotating call cycle of a “pre-call,” “on-call,” and “post-call” team. No patients are admitted to the “post-call” team.
Recently (as of April 2023), UIHC geo-localized all of the inpatient services. This means all general medicine teaching team patients are now almost entirely located on the same floor – just a couple steps from the team room. This also provides for great continuity of care as our residents now work with the same set of nurses, social workers, pharmacist, physical therapists, and occupational therapists, which allows our residents to work together more closely with the support staff and learn from them as they provide outstanding patient care.
There is also an ultrasound machine on the general medicine floor that is easily accessible and readily available for point-of-care ultrasound exams and performing bedside procedures.

Iowa City VA Inpatient Medicine
The Iowa City VA Medical Center is a 3 minute walk away from UIHC and it provides a fantastic learning opportunity for residents. Patients come from a wide range of socioeconomic status’ and backgrounds and they present with a wide variety of medical problems, that range from “bread and butter medicine” to the “zebras”.
The ICU at the VA is also an open ICU that is staffed with a pulmonary/critical care staff and fellow, which allow our residents to get experience taking care of all levels of acuity.
Three teams, each comprised of a staff hospitalist, one senior residents, two interns, a pharmacist, and 2-3 medical students admit, diagnose, and manage the patients admitted for primary medicine problems to the VA. Admissions are allocated based on a rotating call cycle of a pre-call,” “on-call,” and “post-call” team. No patients are admitted to the “post-call” team. The interns work schedule is a rotating schedule with interns covering three days in a row on the pre-call, on-call, post-call cycle. Then the intern transitions to nights and covers the night call shift into the post-call day before starting the call rotation back on days. Overall, interns do an overnight call every 6th night.
Cardiology Inpatient Teaching Service
Comprised of a staff Cardiologist, a senior resident, and two interns, the inpatient cardiology team diagnoses and manages patients with acute cardiovascular illness who do not require an ICU admission. Common problems seen on this service include acute coronary syndromes, decompensated heart failure, valvular disease, pulmonary hypertension, pericarditis, and endocarditis. The team admits patients daily. Overnight, cross-coverage and new admissions are managed by our night float team.

Medicine/psychiatry unit
The medicine/psychiatry unit at UIHC is a 15 bed unit. Residents on this rotation get experience managing the complex interactions between psychiatric and medical illnesses. One team, comprise of a Medicine staff and Psychiatry staff, one senior resident, and two interns care for up to a total of 15 patients who have both a medical indication for hospitalization and a psychiatric indication for hospitalization. The team admits patients daily with no overnight call. Overnight admissions and cross cover are provided by the night float team.
If you are interested in a combined Internal Medicine and Psychiatry Residency, please visit their residency page: https://gme.medicine.uiowa.edu/internal-medicine-psychiatry-residency
Medical Intensive Care Unit (MICU)
The UIHC Medical Intensive Care Unit (MICU) is a 26 bed unit. Common problems managed in the MICU include sepsis/shock, acute and chronic respiratory failure, and other critical conditions.
Two teams, each comprised of a Pulmonary/Critical Care staff, fellow, and 2 senior residents, 1 intern, and 1 APP help provide care to the patients admitted to the MICU. The intern on the team gains experience taking care of critically ill patients by helping to admit patients and provide cross-coverage every other night. Interns do not have any day coverage responsibilities in the MICU. The senior residents take call every fourth night with one day off per week.
Throughout this rotation, residents will have plenty of opportunity to perform beside procedures including central line placement, paracentesis, thoracentesis, lumbar puncture, and arterial line placement. Point-of-care ultrasound is a highly emphasized aspect of this rotation and residents have ample opportunity to get hands on experience obtaining images and measurements at bedside.

Cardiovascular Intensive Care Unit (CVICU)
The UIHC Cardiovascular Intensive Care Unit (CVICU) is a 24-bed unit. Common problems seen on this service include cardiogenic shock, STEMIs, severe valvular dysfunction, and life-threatening arrhythmias.
Patients admitted to the CVICU are either admitted to the medical team, if their primary problem is a medical cardiovascular problem, or to the surgery team. Four senior internal medicine residents help staff the medical team of the CVICU, along with a staff cardiologist and cardiology fellow. Each resident takes call every fourth night with one day off per week.
During their rotation on the CVICU, residents will become comfortable with the interpretation of hemodynamic monitoring number from PA catheters (Swan-Ganz catheters) and the management of cardiac assist devices including intra-aortic balloon pumps (IABPs) and impellas.

Night Float
The night float team consists of two pairs of one intern and senior resident. Each pair works every other night. This team helps to cross-cover and admit to the Inpatient Cardiology Teaching Service and the Medicine/Psychiatry Unit. The senior resident also covers Surgical co-management (general medicine) consults.
Elective Rotations
The elective rotations allow for residents to spend a dedicated 2- to 4-week block time immersing themselves in a specific sub-specialty to explore their future career interests and deepend their knowledge in the core subspecialities of medicine.
We also have many medicine-adjacent rotations that residents rotate on to explore their other interests.
Subspecialty consult and clinic services:
- Allergy/Immunology
- Acute care clinic
- Cardiology
- Endocrinology
- Gastroenterology
- Geriatrics
- Hepatology
- Hematology
- Infectious Disease
- Oncology
- Palliative care
- Pulmonology
- Nephrology
- Rheumatology
- Surgical-co management (general medicine consults)
Unique clinical opportunities:
- International Health (link to international health page)
- Addiction medicine
- Anesthesia
- Bone marrow transplant (primary service)
- Dermatology
- Hospitalist rotation
- Malignant hematology (primary service)
- Neurology stroke service (primary service)
- Sports medicine
- Transplant hepatology
- Transplant nephrology (primary service)
- Visiting resident at a hospital outside the VA and UIHC
Unique opportunities beyond patient care:
- Research elective
- Teaching resident rotation
- Course on EKG interpretation
- Health informatics
Hospitalist Rotation
The hospitalist rotation pairs residents interested in hospitalist medicine with a staff working on a “hospitalist only” service. We have a partnership with St. Luke’s hospital in Cedar Rapids, so residents have the opportunity to experience the day-to-day workflow of a hospitalist firsthand in either a community or academic setting, if the resident wished to stay a UIHC.
Y-Week
During the Y-week, our residents learn the key skills of taking care of patients in the outpatient setting. Residents participate 5 half days of Continuity of Care Clinic, 2 half days in a subspecialty clinic, 1 half day dedicated to working on their quality improvement curriculum, 1 half day of administrative time, and 1 academic half day dedicated to resident education.
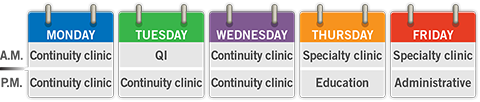
Continuity of Care (COC) Clinic
Residents spend five half days in their Continuity of Care (COC) Clinic at the VA or IRL. This clinic presents an opportunity to build personal panel of patients over 3 years of residency. Residents are responsible for acute clinic problems, chronic disease management, and preventative care.
Residents can also elect to spend a half day in the Iowa City Free medical clinic or the LGBTQ clinic as one of their 5 COC clinic days.
Specialty clinic
Residents rotate in 2 different subspecialties. Subspecialities that match the residents career goals and interests are prioritized. Residents often work with the same staff during their Y-week specialty clinic, which allows for the development of a mentor-mentee relationship between staff and residents. Residents interested in research often end up doing research with their Y-week subspecialty staff or end up being connect to a research project by their Y-week subspecialty staff.
Quality Improvement half day
Every resident participates in a group QI project. The group that you work with is your Y-week cohort. During each Y-week, there is a half day scheduled for the resident to work on tasks related to their QI project.
Administrative half day
This is time set aside in your schedule to catch up on the administrative tasks of being in clinic. Residents use this time to finish up notes and call patients with results. Many residents also use this time to catch up on things outside the hospital like haircuts, dental appointments, and going to see their own doctor.
Academic half day
This is when residents participate in Ultrasound Curriculum, Quality Improvement, Resident Teaching Skills Curriculum, Board Review Curriculum, RRT/Code Blue Simulation, and Ambulatory Workshops.
It’s also a great time to spend time with your co-residents.
For more information about the education half day or the curriculum mentioned above, please visit the Residents as Learners section.
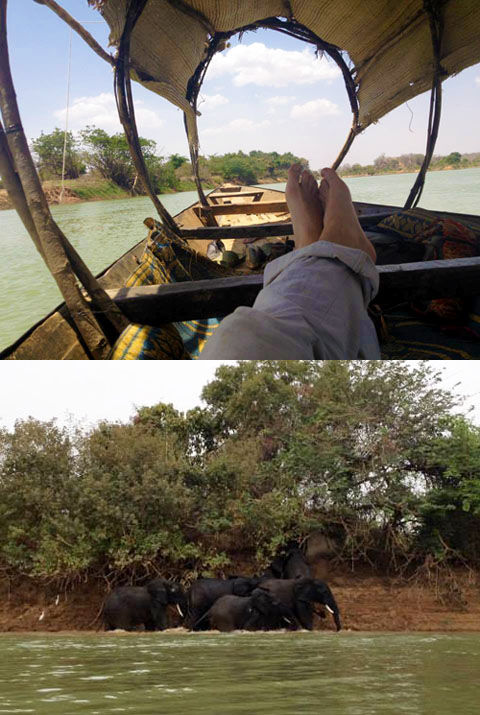
International Health
The Internal Medicine Residency at Iowa offers international health rotations through our international partners. These rotations are intended to give the participating residents a more global perspective in cultural, social, economic, and political issues of another country that impact the nation’s healthcare system. Two of our residents will be participating in an international health rotation in Uganda, mentored by Dr. Robert Blount, in February of 2024. This will be our first international health rotation since COVID!
We also have established connections in India, Ghana, and Niger. You can read about our residents experiences at these sites from pre-COVID times below.
For questions regarding an international health rotation during residency, please contact the Residency Program at intmedres@uiowa.edu.
Dr. Maria Story: "I went to Lady Willington Hospital in Manali, India during my third year of residency for 4 weeks. Manali is a rural hill station (small town) in the state of Himachal Pradesh in north central India."
Dr. Josiah Zubairu: I spent 2 weeks in the village of Agbozume, Volta Region in Ghana in the Spring of 2017 during my 3rd year of residency. This was my second time visiting and providing healthcare to this community of mostly farmers and traders.
Dr. Juan Caraballo: I spent the last 3 weeks and a half in Niamey, Niger. Niger is a landlocked country in West Africa. I worked under the supervision of Dr. Susan Beebout in the Clinique Olivia, a clinic in a poor part of the city associated with Evangelical Church of Niger.
India International Rotation
I went to Lady Willington Hospital in Manali, India during my third year of residency for 4 weeks. Manali is a rural hill station (small town) in the state of Himachal Pradesh in north central India. The Lady Willingdon Hospital is a Christian mission hospital that has been serving the local community since 1935. The catchment area is extremely broad, serving patients up to 10 hour drive on poor quality mountainous dirt roads since there is minimal medical infrastructure in the this area (Himalayan Mountains).
I stayed on the hospital campus (they have small rooms available for rotating trainees) and there were several students from the UK also doing an elective rotation. In the morning we did hospital rounds on infants and children, patients hospitalized for medical conditions, and post-surgical patients. In the late morning and through the afternoon we did outpatient clinic, which was essentially an acute care clinic. There is very little chronic disease management or focus on health prevention. Basic laboratory testing and X Rays were available when absolutely indicated. There is also a labor and delivery room (which I did not participate much in, given that I was an Internal Medicine trainee) and an 24-hour Emergency Department.
I saw a wide variety of illnesses, including TB, Scrub Typhus, Entamoeba histolytica, dysentery, a variety of worm infections, and typical bacterial pathogens. There was a high number of accident-related injuries, primarily from MVA’s and unsafe work conditions. Older people presented with respiratory symptoms, probably from some form of obstructive lung disease from smoke exposure from cooking fires and inhaled dust/dirt from hard labor.
Throughout my elective, I was impressed that the staff at Lady Willingdon Hospital were able to provide excellent care with minimal resources by our standards. I did experience a degree of ‘culture shock,’ but overall it was a very valuable experience and I am thankful for the opportunity to travel to India during residency. I felt safe throughout my time in Manali, the scenery was amazing, and I had the opportunity to meet many wonderful people.



Ghana International Rotation
I spent 2 weeks in the village of Agbozume, Volta Region in Ghana in the Spring of 2017 during my 3rd year of residency. This was my second time visiting and providing healthcare to this community of mostly farmers and traders. It was very positive experience for exposure to clinical work, community education and understanding disparities in healthcare access. I was exposed to multiple array of interesting pathology and medical cases, some with very limited resources for further evaluation and management. I had to make grasp of whatever limited options I had to pursue care of these people. Exchanging ideas with local physicians and people in the community was also very educative. I plan to continue to visit Agbozume.
I am thankful that the medicine department could support me in many ways for my trip to Ghana. I will encourage many others with interest in International Health to consider this tremendous opportunity.

Niger International Rotation
I spent the last 3 weeks and a half in Niamey, Niger. Niger is a landlocked country in West Africa. I worked under the supervision of Dr. Susan Beebout in the Clinique Olivia, a clinic in a poor part of the city associated with Evangelical Church of Niger. During my time in Niger I had the unique opportunity to work with an underserved population and with limited resources. I had the opportunity to see and help a broad spectrum of patients with a broad spectrum of pathologies, including diabetes and hypertension, typhoid, tuberculosis, sickle cell disease and many more. I would see around 10-12 patients daily with the help of a medical assistance that will also serve as translator. Most patient speak only their native language (Hausa, Zarma) and only around 20% speak French. Only very limited labs were available and most patients were not able to afford extensive diagnostic work up.

Practicing in an environment where laboratories test and imaging are not readily available I learned to trust my history taking and physical exam, and to formulate a clinical assessment with just limited information. Having to serve a population with limited resources strengthen my resourcefulness and taught me about cost-effectiveness in a very direct and practical way.

During my rotation in Niger I had the opportunity to spent one week at the National Hospital of Niamey, where I was part of the team taking care of 32 patients in the women general ward. I learn about the logistics of patient care and education in a teaching hospital and the day to day life of my colleagues residents in Niger. Even though the National Hospital is one of the main three hospitals in Niamey, the capital of Niger, there are no ventilators, angiography or MRI, and most medications routinely used in US are not available there, at all. Being able to see the highest level of care that is available in one of the poorest countries in the world, compared with United States, was a humbling and enlightening experience that I feel fortunate to have had and I m positive it has enriched me no only professionally but personally.
LGBTQ Clinic
Our residents can elect to provide care in the LGBTQ clinic in the place of one of the half days of Continuity of Care clinic. The LGBTQ clinic provides welcoming and affirming care for all patients. Residents in this clinic learn about the unique aspects of providing healthcare to the LGBTQ population while also learning about the challenges faced by the LGBTQ population from across the state of Iowa and how this affects their access to healthcare.
Please check out the LGBTQ clinic website for more information.
Iowa City Free Medical Clinic
Our residents can elect to provide care in the free medical clinic as one of their five half days of Continuity of Care clinic. Residents who rotate at the free medical clinic get first hand experience in helping the underserved communities in the Iowa City area and learning about the challenges they face in accessing healthcare.
Please check out the Free Medical Clinic website and the Distinction in Health Equities.
MAT Clinic
Residents can care for people with substance use disorders (SUD) by electing the Medications for Addiction Treatment (MAT) clinic as one of their elective or continuity clinic experiences. Residents who spend time in the MAT clinic get clinical exposure in starting and managing evidence-based medications for SUD. They will support patients through early and established recovery, screen and treat for concurrent medical and psychiatric comorbidity, and advocate for patients as they intersect with other non-healthcare institutions encountered by people with SUD.
Preliminary Year
A one-year program is available for candidates who require Internal Medicine training prior to starting another specialty. We treat our preliminary residents the same as we do our categorical residents. Our prelims participate in the same orientation as our categorical residents, they are invited to all of our didactic conferences, and all of our residency’s social events outside of the hospital. The year culminates with a graduation ceremony that celebrates the 3rd year categorical residents’ graduation and also our prelims graduation as they move on from the IM program to their respective specialty of choice.
We also work with our prelims to individualize their schedule as much as possible to maximize the applicability of their rotations to their future career specialty. The major difference between the prelim schedule and the categorical schedule is there is no Y-week, only 4 week blocks of rotations.
For more information on our prelim year, please reach out to intmedres@uiowa.edu.
Internal Medicine-Psychiatry Residency
 The Internal Medicine and Psychiatry Combined Residency Program at the University of Iowa is a 5-year program that offers residents the opportunity to provide comprehensive care to patients with comorbid medical and psychiatric conditions.
The Internal Medicine and Psychiatry Combined Residency Program at the University of Iowa is a 5-year program that offers residents the opportunity to provide comprehensive care to patients with comorbid medical and psychiatric conditions.
Educational Experiences
At Iowa, we are dedicated to providing case-based, framework-focused didactic sessions and workshops that helps to supplement and accelerate our residents’ growth as clinicians. We do this through a variety of educational environments and distinct curricula.
We also currently offer two pathways and three distinction tracks (with hopes of adding more in the future) that give residents the opportunity to individualize their education and explore topics that interest them in a more in-depth manner.
Please explore the variety of learning environments, curricula, pathways, and distinction tracks we offer at the University of Iowa.
For information on research opportunities while in residency, visit the “Residents as Scholars” section.
Learning Environments
All didactic sessions take place on a regular schedule that all faculty are aware of. This facilitates residents getting to conference on time and having a dedicated time for teaching in their daily schedules.
Noon Conference
From 12:00-1:00pm every Monday, Tuesday, Wednesday, and Friday (Thursday is Grand Rounds), all internal medicine residents and prelims on IM rotations gather in our lecture room for a didactic session. See the curricula below to see examples of what we learn about.
FREE FOOD IS PROVIDED! You don’t even have to use your call money.
Pagers are monitored by our wonderful administrative page. If you get a page that needs to be addressed urgently, they will let you know. Otherwise, noon conference time is a break in the day dedicated to learning.
While you are in the food line is a great time to socialize with your co-residents.
Morning Report
Morning report is led by residents for residents. Every Wednesday from 7:15-7:45, a resident presents a case to the other residents on elective rotations to hear a case presentation. Chief residents help add to the teaching points brought up by the resident presenter.
Recent morning report cases:
- Fanconi syndrome due to oxaliplatin
- Discussion point 1: Physical exam findings to differentiate venous stasis from lymphedema
- Discussion point 2: Differentiating between the RTA type 1, 2, and 4
- Native-valve endocarditis leading to hemorrhagic stroke and altered mental status
- Discussion point 1: Framework for altered mental status
- Discussion point 2: Physical exam findings of endocarditis
- Air embolism leading to chest pain and stuttering speech
- Discussion point 1: Framework for chest pain in a patient with cancer
- Discussion point 2: Prevention and management of air embolism
Academic half day
On Thursday’s from 1:00-5:00pm on residents’ Y-week, residents participate in a variety of interactive didactic sessions. Depending on the week, residents will either be participating in the Ultrasound curriculum, RRT/Code blue simulation curriculum, Quality Improvement curriculum, Resident teaching skills curriculum, or Board review.
Additionally, each academic half day ends with an ambulatory workshop. The ambulatory workshop is an interactive session on a topic particularly relevant to primary care.
Topics covered recently include:
- Shoulder MSK physical exam and practicing shoulder injections
- Knee and ankle MSK physical exam and practicing knee injections
- Men’s health – BPH, ED, hypogonadism
- Women’s health – breast cancer screening and common breast problems
- LGBTQ+ health, health inequities, implicit bias
- Motivational interviewing for addressing substance use and obesity
- Anorectal disease and practice anoscopy
- Dermatology basics and practice skin biopsy
Master clinician rounds
Every Friday, from 8:00-8:30 the long call team presents one of their patients that they currently have on service to a master clinician (AKA our program director Dr. Suneja) and the chief residents, none of whom know the final diagnosis. As the case unfolds, the master clinician discusses their thought process as it applies to the case. After the presentation, the team and master clinician examines the patient and demonstrates relevant physical exam findings.
Internal Medicine Grand Rounds
On Thursday from 12:00 – 1:00, the whole internal medicine department gathers for grand rounds. Grand rounds are organized by the department of internal medicine. Topics are often focused to updating primary care providers and general internists to developments in the subspecialties.
Food is provided to all attendees, including residents!
Recent talks include:
- “Updates in Alcohol” by Dr. Andrea Weber
- “Osteoporosis in Patients with Anorexia Nervosa” by Dr. Amal Shibli-Rahhal
- “Rural Health: What it means for the VHA, UIHC, and the Nation” by Dr. Peter Kaboli
- “Death from Asthma” by Drs. Gregory Schmidt, Eyas Azayadneh, and Zeke Quittner-Strom (an internal medicine resident!)
Curricula
Core Topics in Internal Medicine
The majority of noon conference topics fit under this curriculum. We emphasize having a curriculum that is interactive and case based. We cover topics from all subspecialties of internal medicine (and beyond) that are relevant for general internists and primary care doctors.
Highlights from this series include:
- The “Emergencies” lectures: Infectious disease emergencies, endocrine emergencies, dermatologic emergencies, and psychiatric emergencies to name a few
- “Pancreatic cystic lesions”
- “Buprenorphine 101”
- “Breast cancer for the internist”
- There are also disease focused talks, like “Acute pancreatitis” and “Chronic Obstrucive Pulmonary Disease” other important talks like that
Ultrasound curriculum
For more information, go to Ultrasound Curriculum.
Quality improvement curriculum
For more information, go to Quality Improvement Curriculum.
Clinical Reasoning Curriculum
For more information, go to Clinical Reasoning Curriculum.
Framework Fridays
Introduced in 2023, Framework Friday’s are case presentations led by the chief residents during noon conference that dive deeply into a framework and how applies to clinical reasoning related to the case.
Topics covered include:
- Shortness of breath
- Hemolytic anemia
- Microcytic anemia
Master Clinician Mystery Case Series
The Master Clinician Mystery Case Series was developed by residents Luke Morrey and Rachel Genova (’23) as part of a Distinction in Medical Education (link) curricular project. For this series, a case is presented to a master clinician in aliquots and the attendees break into small groups and discuss their approach to the case before coming back as a group to hear what the master clinician is thinking as the case unfolds. The emphasis is on reasoning and the correlation between basic pathophysiology and clinical presentation.
Topics covered include:
- Pulmonary-renal syndrome
- Lactic acidosis
- Interstitial Lung Disease
RRT/Code Blue Simulation
Residents participate in simulations of Rapid Response and Code Blues during the ambulatory curriculum of their Y week. This is a progressive learning experience with the PGY2s running the simulation, the PGY1s assisting and the PGY3s giving feedback. This was an addition to the educational opportunities made available to residents during the 2023-2024 academic year and it has been very well received.
Board review curriculum
Board review is a longitudinal curriculum that occurs during the academic half day of Y weeks and during noon conference in the later part of the year. Additionally, our program facilitates a “Board Review Weekend” at the end of the academic year for graduating residents. These didactic sessions are organized around MKSAP questions and focused on content heavily covered by the ABIM in order to reinforce clinical reasoning, key points, and test taking strategies.
Resident Teaching Skills Curriculum
For more information, go to the Teaching Skills curriculum.
Wellness curriculum
For more information, go to Wellness Curriculum.
Health Equity Curriculum
Introduced in spring of 2023, the purpose of the Health Equity curriculum is to increase residents’ awareness of issues of health equity within medicine and give residents tools to minimize them. These talks are given during noon conference on a regular interval to increase our residents training in this critically important issue. For residents learning more about health inequities in medicine, we also offer a Distinction in Health Equity as well as clinical experiences in the Free Medical Clinic and LGBTQ clinic.
Talks given in this series include:
- “Health equity and disparity”
- “Stigma and evaluation in substance use”
R2 Talks
All second-year residents participate in creating and delivering a noon conference lecture and handout on an educational topic of their choice. Residents are paired with faculty mentors and given feedback.
Talks given by residents include:
- “Alcohol-associated hepatitis”
- “Infective endocarditis: beyond the TEE”
- “Pulmonary Langerhans Cell Histiocytosis”
- “Clinical diagnostic errors”
Journal Club
All third-year residents lead a discussion of a current primary literature in internal medicine or internal medicine subspecialties. There focus is on critically appraising the study design and evaluating the applicability of these results to patient care.
Ultrasound Curriculum
The Point-of-Care Ultrasound (POCUS Curriculum) is a longitudinal, integrated, and progressive learning experience that teaches bedside ultrasonography and how it can be utilized in patient care. This curriculum is taught during the academic half day of the Y-week. This curriculum focuses on hands-on scanning of simulated patients with in-person faculty mentors who provide real-time feedback.
Here are some example modules:
| Basic POCUS Modules (PGY-1) | Advanced POCUS Modules (PGY-2 and above) |
|
|
Quality Improvement Curriculum
The Quality Improvement curriculum at the University of Iowa is an integrated curriculum that incorporates workshops during the academic half day of the Y week and a year-long team-based quality improvement project designed and implemented by the Y week cohorts.
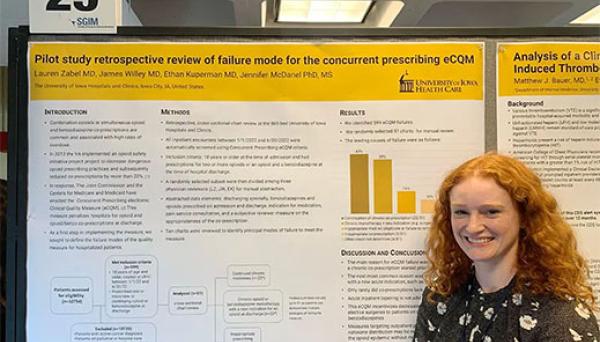
The University of Iowa Hospitals and Clinics hosts an annual Quality and Safety Symposium in which our resident teams are given the opportunity, encouragement, resources, and mentorship to submit and present their projects. After this, many teams submit their projects to large regional and national meetings.
Since the development of our curriculum we have had…
- 50+ resident led QI Projects
- 30+ resident led QI Projects presented at our local Quality and Safety Symposium (link)
- 25 resdient teams presented oral presentation or posters at SGIM Midwest Regional Meeting
- 7 resident teams presented posters at SGIM National Meeting
Our groundbreaking curriculum was published in the Journal of Graduate medical Education.
Example QI projects:
- Naloxone prescription for opioid use disorder
- Hepatitis C screening
- Patient-Provider Communication – AVS summary use at the VA
- SGLT2 prescription for CKD
Clinical Reasoning Curriculum
One of the highlights of our program’s curricula is the emphasis on clinical reasoning. Clinical reasoning is a unifying theme of all that we teach here at the University of Iowa. But clinical reasoning takes the spotlight during clinical reasoning week, where Dr. Suneja (our program director) and company take a deep dive into the inner workings of the thought processes of master clinicians. We discuss the nuts and bolts of problem representation and how to form an effective assessment. We then use that problem representation and show how that interacts with frameworks, which ultimately lead to a differential diagnosis. We also discuss cognitive bias and how clinicians are continuously learning and incorporate this new information into their thought processes.
Topics covered include
- “Clinical Reasoning: Thinking of blinking”
- “Speaking the same language and steps to clinical reasoning”
- “Clinical Reasoning: Novice to Expert”
Additionally, the primary focus of Morning Report, Master Clinician Rounds, Framework Friday’s, and Master Clinician Mystery Case series is clinical reasoning. All of these experiences work together to develop our residents clinical reasoning skills over their three years of residency.
Wellness Curriculum
The wellness curriculum covers a wide spectrum of issues related to wellness. The talks are selected and organized by the Wellness and Humanities Committee. Some of the favorite talks from this series are the yearly two-part talk on personal finance and the faculty panel on dealing with errors.
Wellness talks during noon conference include:
- “Sleep during residency”
- “Financial wellness” – a 2 part lecture series
- Faculty panel on dealing with errors and patient death
- Our yearly Pumpkin Carving Contest and Holiday party with cookie decoration that happen over noon conference
Distinction Tracks
Our residency offers three distinction tracks that expand upon content that is taught in other parts of our residency’s curriculum. These distinction tracks meet on a monthly basis during the noon hour and discuss topics relevant to their distinction.
A crucial aspect of each of the distinction tracks is mentorship and a scholarly project. Scholarly projects give residents an avenue to apply what they learn in the distinction track meetings and mentors identified through the distinction track provide regular guidance.
Distinction in Health Equity (DIHE)
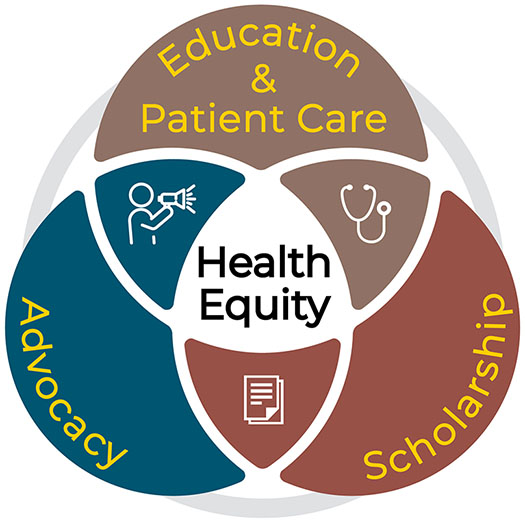
The Distinction in Health Equity (DIHE) track is designed for residents who envision working towards eliminating disparities in health care as part of their professional career. Residents participating in the DIHE are immersed in a flexible, mentored, experience-based curriculum with hands-on activities in a variety of low-resource settings. This curriculum is specifically designed to go beyond the health equities curriculum that is taught during noon conference to all internal medicine residents. Residents who participate in the DIHE will also complete a capstone project that addresses a health equity need.
This track was first introduced in the fall of 2022.
2024 DIHE Participants

Rachel Anderson

Adam Blaine

Calie Brownlee

Paige Carlson

San Chandra
Katrina Dovalovsky

Cole Howie

Sarah Little
Kimiya Nourian

Shivali Patel

Laurel Smeins

Katrina Soyangco

Alice Xu

Lauren Zabel
Leadership

Krista Johnson, MD, MME

Jeydith Gutierrez, MD, MPH

Desmond Barber, MD

Manish Suneja, MD

Denise Floerchinger
Distinction in Medical Education (DIME)
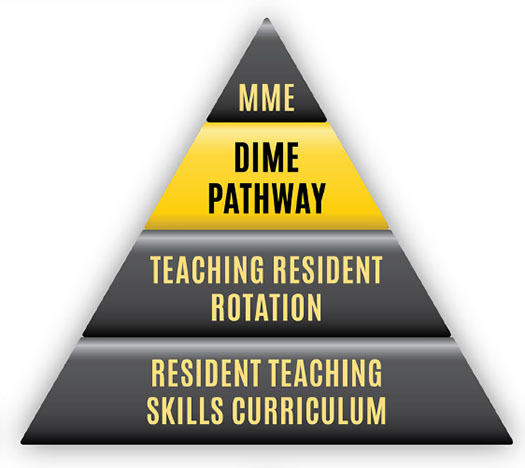
The Distinction in Medical Education (DIME) track is designed for residents who are interested in becoming clinician educators and who wish to include medical education as part of their profession career. The DIME curriculum provides experiences and further educational instruction beyond the current three-year longitudinal resident teaching skills curriculum by focusing on curriculum design and development, educational innovations, and educational scholarship. Each resident in DIME works with a mentor on a scholarly project.
Some example projects include:
- Curriculum development for the Transition to Residency course offered to fourth year medical students at the University of Iowa Carver College of Medicine. Workshops developed by DIME residents included workshops on hypoxia, chest pain, and altered mental status
- The Clinical Unknown Series
- Introduction to Medicine Workshop for Under-Represented High School Students
- Core Physical Exam Technique Simulation for Internal medicine Clerkship Students
- Medicine workshop series
Residents have presented their scholarly projects at local and national meetings.
Both the Master Clinician Mystery Case series and the Distinction in Point-of-Care Ultrasound stem from work done as a part of the Distinction in Medical Education.
2024-2025 DIME Participants

Grace Alexander

Calie Brownlee

Stefano Byer

Amanda Chang

Nick Coffey
Katrina Dovalovsky

Brittnee Haynes

Alp Kahveci

Tyler Maggio

Shivali Patel

Megan Napier

Joe Phillips

Pranav Puri

Ashten Sherman

Carlie Sorensen

Katrina Soyangco

Quinn Vatland

Alice Xu
Leadership

Jenny Strouse, MD
Director

Yana Zemkova, MD
Co-Director

Stacy Sueppel
Administrator
Steering Committee

Manish Suneja, MD

Lisa Antes, MD

M. Lee Sanders, MD
Distinction in Point-of-Care Ultrasound
The Distinction in Point-of-Care Ultrasound track is designed for residents who are interested in an advanced educational experience in point-of-care ultrasound (POCUS) and who anticipate utilized bedside clinical ultrasound as a part of their professional career. Residents who participate in this distinction are immersed in a flexible, mentored, experienced-based curriculum with hands-on learning and teaching activities specifically designed to extend beyond the current three-year longitudinal resident ultrasound curriculum (link to Ultrasound Curriculum accordion in the Curricula subsection). Residents work with mentors who review the portfolio of images obtained by the resident at bedside and provide feedback. Residents will also complete a scholarly activity related to ultrasound and/or ultrasound education under the guidance of their mentor.
This distinction track was first introduced in the Fall of 2022.
Leadership

Fellow Director: Sydney Bowmaster

Faculty: Justin Smock

Faculty: Charles Rappaport

Administrator: Abbey Gilpin
2023 POCUS Participants

Grace Alexander

Rachel Anderson

Adam Blaine

Paige Carlson

Solanus de la Serna

Hunter Frederiksen

Sruti Prathivadhi-Bhayankaram

Haley Pysick

Michael Sauer

Ashten Sherman

Mike Shlossman
Pathways
Our residency offers two pathways that are tailored to residents interested in primary care or hospitalist medicine.
Primary Care Pathway
The Primary Care Pathway is a flexible program designed to provide clinical experiences and education that support residents in the pursuit of excellence in primary care. As part of the pathway, residents are invited to attend educational sessions over the noon conference hour that focus on different aspects of primary care like the similarities and differences between community and academic primary care, billing in primary care, and how to go about a job search for primary care physicians. Residents in the primary care pathway are given scheduling priority for rotations that prepare them for primary care like sports medicine, dermatology, women’s health, and the Medication-Assisted Treatment (MAT) clinic. Residents are also paired with a mentor who shares similar interests and career goals to help them as they work through this pathway.
Hospitalist Pathway
The Hospitalist Pathway is designed for residents who wish to prepare for a career in inpatient general medicine. As part of this pathway, residents are given priority in scheduling career specific rotations like the stroke team and the hospitalist elective, which is a one-on-one experience with an experienced hospitalist on a non-teaching service. Residents also attend conferences hosted over the noon hour where hospitalists discuss topics like inpatient billing, health care delivery systems, patient safety, and how to go about doing a job search for hospitalist positions with the residents.
Residents as Educators
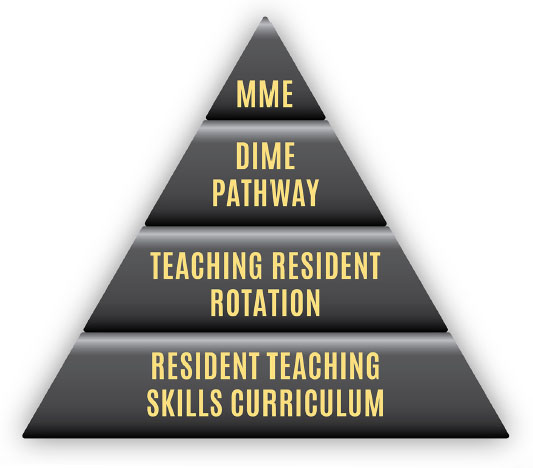
At the University of Iowa Internal Medicine Residency Program, we believe becoming a skilled educator is crucial to your development as a physician. Our residents spend a significant portion of their time on the wards teaching medical students. Additionally, the teaching skills our residents develop aid in their development as clinicians because the doctor-patient relationship is in large part a teaching relationship. After all, the word “doctor” comes from the Latin word that means “to teach.”
In an effort to help residents develop teaching skills, residents will be given ample opportunity to assume the role of teacher throughout their time as a resident. All residents also participate in our three-year, longitudinal teaching skills curriculum.
For residents interested in making education a larger part of their future career, we also over the Distinction in Medical Education track and the opportunity to pursue classwork towards obtaining a Masters in Medical Education.
Teaching Awards
Talks Given by Residents
Throughout their 3 years of training, our residents have numerous opportunities to teach.
Teaching medical students
Whether its informal teaching points in between patients on rounds, while walking to see a new admit in the ED, or a chalk-talk in the team room, most of our residents teaching time will be spent teaching students.
R2 talk
During the R2 year, our residents prepare a 30-minute presentation on any topic within internal medicine, ranging from Pulmonary Langerhans cell Histiocytosis to Clinical Reasoning Errors. These presentations are prepared under the direction of a resident-chosen mentor who helps provide feedback.
Journal Club
During the R3 year, our residents prepare a 30-minute presentation on a recent ground-breaking study in the field of internal medicine. The leading resident walks their peers through the study design and results and discusses the impact of this article on current practice.
Morbidity, Mortality, and Improvement Conference
Anytime during residency, our residents have the opportunity to present a patient case during our MMI conference and discuss the systems issues that negatively impacted patient care.
Morning Report
During the R2 and R3 year, our residents prepare a case presentation for their peers. The presenting resident chooses the teaching points and drives the education of their co-residents forward.
ACP Clinical Vignette
All residents given one or more clinical vignette presentations during our friendly annual ACP clinical vignette competition throughout their residency. The winner of the competition goes on to present at the statewide ACP chapter meeting.
Teaching Skills Curriculum
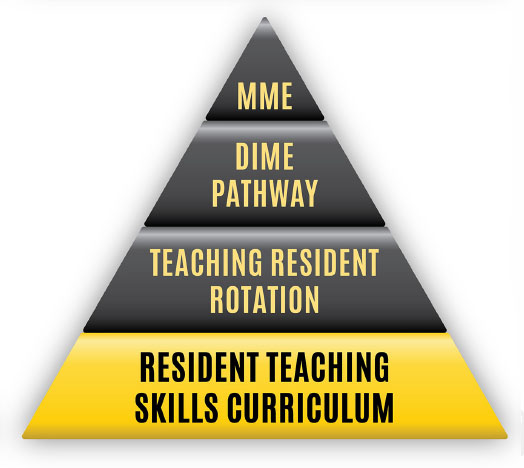
The Teaching Skills Curriculum is a longitudinal, integrated, and progressive workshop-based curriculum that introduces residents to the knowledge base and skill set used when serving in the role of a clinician-educator. This curriculum is taught during the academic half day of the Y-week. This curriculum focuses on skills and techniques that would be used to teach medical students while on rotations like creating an effective learning climate, one-minute preceptorship, and chalk-talk 101.

Teaching Skills Curriculum goals
The goal of the Teaching Skills curriculum is to introduce residents to a knowledge base and skill set used when serving in the role of a clinical educator. The longitudinal curriculum for all residents presents concepts and allows residents to practice skills associated with topics such as establishing the learning climate, motivating the learner, one-minute preceptor and feedback and evaluation as well as interactive teaching and evaluation.
Sessions are interactive covering a topic related to current best teaching practices. There is time for skill development and through the process of deliberate practice, residents design an action plan for further skill development. Residents complete pre-session readings and following each session are expected to refer to their action plan in teaching encounters.
Session #1: Introduction to Teaching Skills, Learning Climate and Effective Teachers
- identify characteristics of exemplary clinical teachers
- identify strategies to promote an effective learning climate
- demonstrate teaching behaviors that promote an effective learning climate
- develop an action plan to improve the learning climate in your own teaching
Session #2: Motivating the Learner
- examine contributing factors that affect a learner’s performance.
- explain one relevant motivational theory that covers extrinsic & intrinsic motivators.
- discuss the importance and impact of a good orientation.
- identify components of an orientation.
Session #3: One-Minute Preceptor
- describe the 5 elements of the one-minute preceptor model for clinical teaching.
- successfully apply the model to a simulated learner presenting a patient.
- use the model to develop an assessment of the learner’s current level of knowledge/skill and what the learner needs to know.
Session #4: Feedback
- define feedback and give rationale for providing feedback to learners.
- recognize barriers to giving feedback.
- identify characteristics of effective feedback.
- demonstrate effective feedback via observation and practice.
- develop an action plan for improving personal feedback skills.
Session #5: Interactive Teaching/Use of Technology
- know the goals of effective lecturing/presentation.
- describe components of effective lecturing/presentation.
- apply specific techniques for making lectures more interactive.
Session #6: Evaluation of Students, Peers and Faculty
- define evaluation and differentiate it from feedback.
- obtain an understanding of the use of commonly used evaluation tools and techniques.
- gain insight into common pitfalls surrounding evaluations.
- understand why accurate evaluation is important.
Teaching Resident Rotation
Each year, a sub-set of third year residents are selected to be the “Teaching Resident” for a 4-week period. The Teaching Resident is responsible for teaching the core-year and Sub-I medical students on internal medicine rotations in small-group facilitation, interactive classroom lecturing, simulation session, and bedside instruction. This rotation is a fantastic opportunity to demonstrate the skills obtained through participation in the longitudinal Teaching Skills Curriculum. Feedback is provided to each Teaching Resident through written evaluations from the students they taught as well as direct observation by a faculty mentor.

Masters in Medical Education
The Masters in Medical Education (MME) is a competitive, 30 semester-hour program coordinated through the Office of Consultation and Research in Medical Education at the Carver College of Medicine. Learners enrolled in the masters program take seven core courses covering topics including educational measurement in medical education, current issues in medical education, instructional design and technology, teaching methods, clinical teaching, assessment in medical education and educational research and evaluation as well as electives. In addition to coursework, the participant develops a summative portfolio project.
During residency, residents have the opportunity to complete coursework in the MME program and work towards earing a certificate (Medical Education, Graduate Certificate). This coursework will contribute to a Masters of Medical Education if a resident chooses to pursue further studies. The residency will cover the cost of these classes while the student is a resident.
The Masters in Medical Education (MME) program provides residents, fellows and staff the opportunity to develop teaching skills specific to medical education. Guided by the faculty in the Office of Consultation and Research in Medical Education (OCRME), the curriculum introduces learners to different areas of evidence-based assessment and educational principles, and invites participants to contribute to this growing area of research while allowing them to complete a strong portfolio. Classes are physician schedule-friendly with online options or weekly seminars after 5:30 pm. The program timeline is flexible and highly supported by the department of Internal Medicine. I highly recommend this opportunity to any healthcare provider interested in utilizing medical education as a part of his/her career.
Andrea Weber, MD
Medicine-Psychiatry Resident ('17)
Scholarship and Research
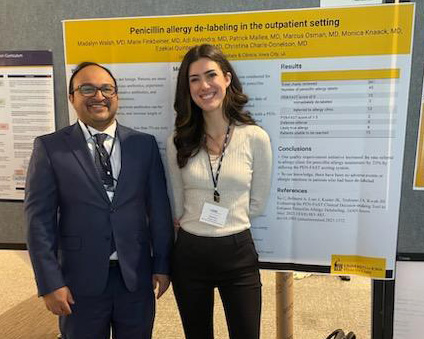
Residents Ady Ravindra and Madalyn Walsh at the 2023 Midwest Society of General Internal Medicine (SGIM) conference
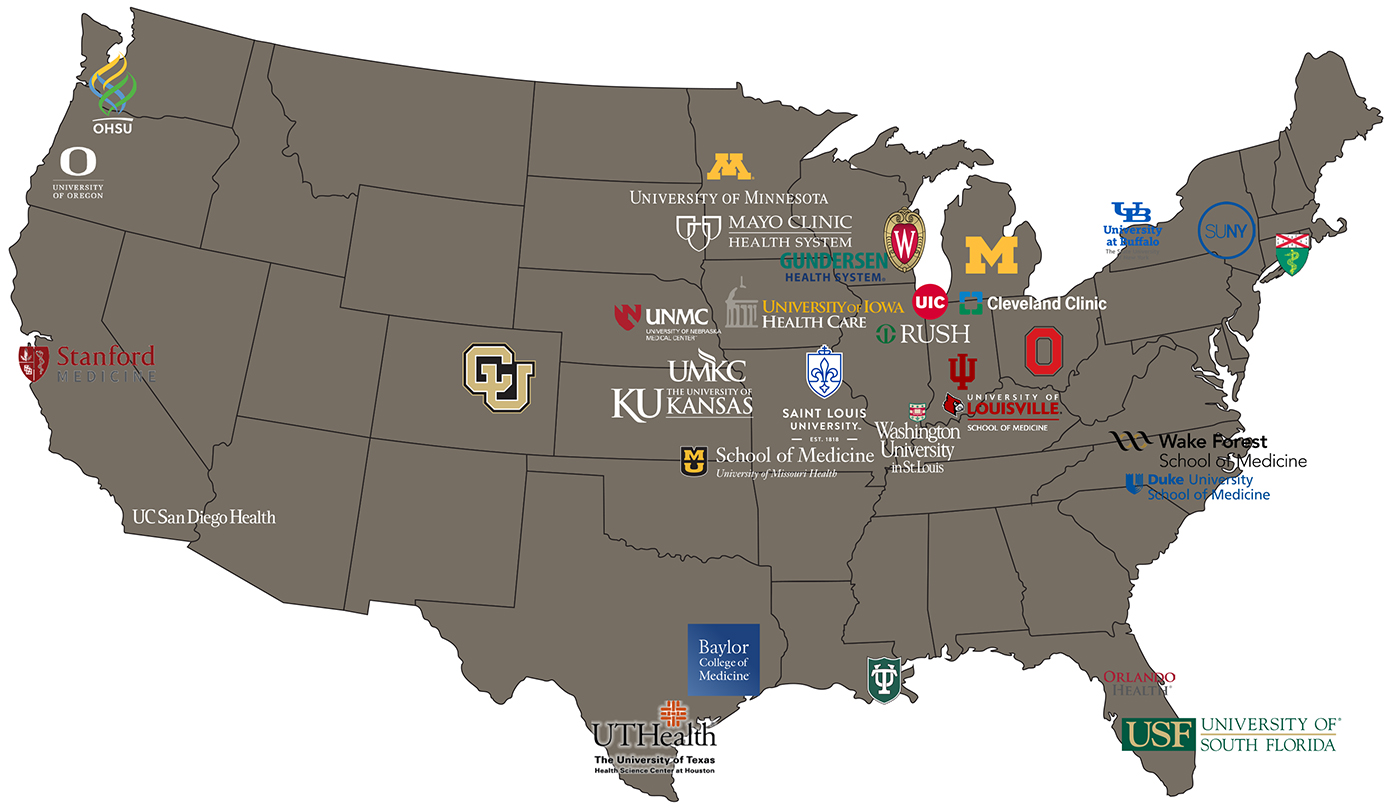
Our residency program will immerse you in scholarship that is informed by your own curiosity. Throughout residency, all of our residents complete at least one scholarly activity. Our residents are provided the opportunity for dedicated research time during their second and third years to pursue scholarship activity. With this culture of scholarship, our residents regularly present their findings at conferences at local, regional, and national levels and publish articles in significant scholarly journals.
For residents interested in making research a larger focus of their future career, we are one of only a handful of residencies nationally that offers the Stimulating Access to Research during Residency (StARR) program and we also offer the Physician Scientist Training Pathway (PSTP).
At Iowa, we recognize that mentorship is a key aspect of helping residents achieve their scholarship goals while in residency. We invite you to learn more about We work to find a good mentor fit that shares your interests.
Scholarship Done by Residents
Throughout residency, all of our residents complete a scholarly activity. At Iowa, we use a broad definition of scholarship that includes all of our residents’ academic interests. The scholarly activity can take the form of a case report, research article, or commentary published in a scientific journal, a poster presentation at a local, regional, or national meeting, or a curricular development project. This is not an exhaustive list. The scholarly activity is flexible and is individualizable to our residents’ interests.
See the list below of journal articles published by our residents from 2018-2023.
Zhang X, Durham KM, Garza AA, Murali AR. Portal vein thrombosis, hepatic decompensation, and survival in patients with porto-sinusoidal vascular disease and portal hypertension. J Gastroenterol. Mar 2023;58(3):268-276. doi:10.1007/s00535-023-01957-0
Zhang K, Zhang J, Robinson T, Saur M, Van Dorin S, Zabel L, et al. Preventing Opioid-Related Toxicity at a Regional VA Medical Center: A Resident-Led Interprofessional Quality Improvement Project. Am J Med Qual. Jan-Feb 01 2023;38(1):68-69. doi:10.1097/jmq.0000000000000100
Zayac AS, Landsburg DJ, Hughes ME, … Saad M… et al. High-grade B-cell lymphoma, not otherwise specified: a multi-institutional retrospective study. Blood Adv. May 12 2023;doi:10.1182/bloodadvances.2023009731
Walsh M, Xu A, Ballas Z, Sanchez R. Disseminated fungal infection in a patient receiving zanubrutinib. Clin Case Rep. Jun 2023;11(6):e7564. doi:10.1002/ccr3.7564
Walsh M, Wasko N, Simms AJ, Hodges J. Splenic abscess caused by Cutibacterium acnes in a patient with multiple tooth extractions. BMJ Case Rep. Jan 25 2023;16(1)doi:10.1136/bcr-2022-250486
Walsh M, Feng A, Lenert P, Kumar B. Tongue necrosis as a manifestation of immune dysfunction: A complex case of systemic lupus erythematosus, histoplasmosis, and macrophage activation syndrome. Clin Case Rep. Jul 2023;11(7):e7735. doi:10.1002/ccr3.7735
Radke SM, Smeins L, Ryckman KK, Gruca TS. Closure of Labor & Delivery units in rural counties is associated with reduced adequacy of prenatal care, even when prenatal care remains available. J Rural Health. Mar 30 2023;doi:10.1111/jrh.12758
Prathivadhi-Bhayankaram S, Abbasi MA, Ismayl M, et al. Cardiotoxicities of Novel Therapies in Hematological Malignancies: Monoclonal Antibodies and Enzyme Inhibitors. Curr Probl Cardiol. Aug 2023;48(8):101757. doi:10.1016/j.cpcardiol.2023.101757
Prakash S, Saavedra R, Lehmann R, Mokadem M. Candy cane syndrome presenting with refractory heartburn 15 years after Roux-en-Y bypass. J Surg Case Rep. Mar 2023;2023(3):rjad130. doi:10.1093/jscr/rjad130
Prakash S, Kinder K, Brown KE. Spleen size change after hepatitis C treatment: a simple parameter to predict clinical outcomes. J Investig Med. Aug 2023;71(6):603-612. doi:10.1177/10815589231171403
Osman M, Koneru G, Weber A. Integrated care models for co-occurring alcohol use disorders and alcohol-associated liver disease in rural communities: Telehealth considerations and opportunities. J Rural Health. Jul 25 2023;doi:10.1111/jrh.12784
Nguyen EK, Suksaranjit P, Bashir MA, Firchau DJ, Gebska MA. Decoding Postinfarction Left Ventricular Pseudoaneurysm. JACC Case Rep. Mar 1 2023;9:101533. doi:10.1016/j.jaccas.2022.07.005
Mhanna M, Sauer MC, Al-Abdouh A, et al. Cognitive behavioral therapy for depression in patients with heart failure: a systematic review and metanalysis of randomized control trials. Heart Fail Rev. Sep 2023;28(5):1091-1100. doi:10.1007/s10741-023-10308-3
Mhanna M, Al-Abdouh A, Sauer MC, et al. Hypothermia as an Adjunctive Therapy in Cardiogenic Shock: A Systematic Review and Meta-Analysis. Ther Hypothermia Temp Manag. Apr 18 2023;doi:10.1089/ther.2023.0005
Melone MA, Becker TC, Wendt LH, et al. Disruption of the circadian rhythm of melatonin: A biomarker of critical illness severity. Sleep Med. Jul 28 2023;110:60-67. doi:10.1016/j.sleep.2023.07.033
Marar RI, Abbasi MA, Prathivadhi-Bhayankaram S, et al. Cardiotoxicities of Novel Therapies in Hematologic Malignancies: Chimeric Antigen Receptor T-Cell Therapy and Bispecific T-Cell Engager Therapy. JCO Oncol Pract. Jun 2023;19(6):331-342. doi:10.1200/op.22.00713
Makrakis D, Bakaloudi DR, Talukder R,… Vather-Wu N… et al. Treatment Rechallenge With Immune Checkpoint Inhibitors in Advanced Urothelial Carcinoma. Clin Genitourin Cancer. Apr 2023;21(2):286-294. doi:10.1016/j.clgc.2022.11.003
Kidder I, Kobayashi T, Ford B, Sekar P. Hip periprosthetic joint infection due to Coxiella burnetii in an adult male. IDCases. 2023;31:e01661. doi:10.1016/j.idcr.2022.e01661
Khan A, Heller E, Alexander G, Hopson J. Better Late Than Never. JACC Case Rep. Mar 15 2023;10:101750. doi:10.1016/j.jaccas.2023.101750
Kamalumpundi V, Rieth J, Tran H, Ashat M, Zhang X. A Case of Erdheim-Chester Disease Causing Secondary Sclerosing Cholangitis. ACG Case Rep J. Jan 2023;10(1):e00963. doi:10.14309/crj.0000000000000963
Hamdeh S, Fathallah J, Zhang H,… Dave D… et al. Predictive Model for Positive Video Capsule Endoscopy in Iron Deficiency Anemia. Dig Dis Sci. Jul 2023;68(7):3083-3091. doi:10.1007/s10620-023-07918-0
Garg A, Garza AA, Goyal S, Lenert P. Rare Case of Remitting Seronegative Symmetrical Synovitis with Pitting Edema Syndrome with Monoclonal Gammopathy of Undetermined Significance. Am J Case Rep. Apr 26 2023;24:e939650. doi:10.12659/ajcr.939650
Evans AZ, Adhaduk M, Jabri AR, Ashwath ML. Is Virtual Learning Here to Stay? A Multispecialty Survey of Residents, Fellows, and Faculty. Curr Probl Cardiol. Jun 2023;48(6):101641. doi:10.1016/j.cpcardiol.2023.101641
Durham K, Zhang X, Xiong Y, Reddy A, Polyak S. Plaque-Like Lesions in the Gastrointestinal Tract. ACG Case Rep J. Aug 2023;10(8):e01115. doi:10.14309/crj.0000000000001115
Bass RD, Phillips J, Sánchez JS, et al. The Ability of Near-Infrared Spectroscopy to Identify Vulnerable Patients and Plaques: A Systematic Review and Meta-Analysis. Interv Cardiol Clin. Apr 2023;12(2):245-256. doi:10.1016/j.iccl.2022.10.006
Anderson CE, Lieberman RA, Olshansky B. Left Atrial Appendage Occlusion Versus Oral Anticoagulation in Atrial Fibrillation. Ann Intern Med. Mar 2023;176(3):eL220516. doi:10.7326/l22-0516
Anderson C, Olshansky B. The LEADR ICD lead study: Is thinner better? J Cardiovasc Electrophysiol. Feb 2023;34(2):268-269. doi:10.1111/jce.15750
Alameddine R, Mallea P, Shahab F, Zakharia Y. Antibody Drug Conjugates in Bladder Cancer: Current Milestones and Future Perspectives. Curr Treat Options Oncol. Jul 5 2023;doi:10.1007/s11864-023-01114-y
Adviento BA, Regan EA, Make BJ, et al. Clinical Markers Associated With Risk of Suicide or Drug Overdose Among Individuals With Smoking Exposure: A Longitudinal Follow-up Study of the COPDGene Cohort. Chest. Feb 2023;163(2):292-302. doi:10.1016/j.chest.2022.09.022
Zandvakili A, Kobayashi T, Kaewpoowat Q, et al. Pelvic and central nervous system tuberculosis complicated by a paradoxical response manifesting as a spinal tuberculoma: a case report. BMC Infect Dis. Sep 24 2022;22(1):750. doi:10.1186/s12879-022-07731-6
Walhof ML, Leon J, Greiner AL, Scott JR, Knudson CM. Hemolytic disease of the fetus and newborn in the sensitizing pregnancy where anti-D was incorrectly identified as RhIG. J Clin Lab Anal. Apr 2022;36(4):e24323. doi:10.1002/jcla.24323
Trepanowski N, Chang MS, Zhou G,… Walsh ME… et al. Delays in melanoma presentation during the COVID-19 pandemic: A nationwide multi-institutional cohort study. J Am Acad Dermatol. Nov 2022;87(5):1217-1219. doi:10.1016/j.jaad.2022.06.031
Talukder R, Makrakis D, Lin GI,… Vather-Wu N… et al. Association of the Time to Immune Checkpoint Inhibitor (ICI) Initiation and Outcomes With Second Line ICI in Patients With Advanced Urothelial Carcinoma. Clin Genitourin Cancer. Dec 2022;20(6):558-567. doi:10.1016/j.clgc.2022.08.006
Talukder R, Makrakis D, Diamantopoulos LN,… Jain J… et al. Response and Outcomes to Immune Checkpoint Inhibitors in Advanced Urothelial Cancer Based on Prior Intravesical Bacillus Calmette-Guerin. Clin Genitourin Cancer. Apr 2022;20(2):165-175. doi:10.1016/j.clgc.2021.12.012
Sun D, Hadjiiski L, Alva A,… Elhag D… et al. Computerized Decision Support for Bladder Cancer Treatment Response Assessment in CT Urography: Effect on Diagnostic Accuracy in Multi-Institution Multi-Specialty Study. Tomography. Mar 2 2022;8(2):644-656. doi:10.3390/tomography8020054
Strouse J, Rajan A, Chang HB, Dimachkie MD, Halbur C, Bettendorf B. Clinical Images: Extranodal Natural Killer/T Cell Lymphoma As a Rare Mimicker of Granulomatosis With Polyangiitis. Arthritis Rheumatol. Mar 2022;74(3):474. doi:10.1002/art.41956
Sternhagen E, Bettendorf B, Lenert A, Lenert PS. The Role of Clinical Features and Serum Biomarkers in Identifying Patients with Incomplete Lupus Erythematosus at Higher Risk of Transitioning to Systemic Lupus Erythematosus: Current Perspectives. J Inflamm Res. 2022;15:1133-1145. doi:10.2147/jir.S275043
Simms AJ, Kobayashi T, Schwartzhoff PV, Sekar P. Prosthetic hip infection due to Campylobacter jejuni. BMJ Case Rep. Mar 10 2022;15(3)doi:10.1136/bcr-2021-248240
Rytlewski J, Brockman QR, Dodd RD, Milhem M, Monga V. Epigenetic modulation in sensitizing metastatic sarcomas to therapies and overcoming resistance. Cancer Drug Resistance. 2022;doi:10.20517/cdr.2021.88
Robl J, Vutthikraivit W, Horwitz P, Panaich S. Percutaneous closure of patent foramen ovale for treatment of hypoxemia: A case series and physiology review. Catheter Cardiovasc Interv. Sep 2022;100(3):471-475. doi:10.1002/ccd.30317
Prescott AE, Ravindra A, Javed A. Neutropenic Enterocolitis: A Rare Complication of Sacituzumab Govitecan. Case Rep Oncol. May-Aug 2022;15(2):687-693. doi:10.1159/000525351
Prakash S, Obeidat M, Murali AR. Colonic Venous Blebs Secondary to Gastrointestinal Amyloidosis. ACG Case Rep J. May 2022;9(5):e00783. doi:10.14309/crj.0000000000000783
Makrakis D, Talukder R, Lin GI,… Vather-Wu N… et al. Association Between Sites of Metastasis and Outcomes With Immune Checkpoint Inhibitors in Advanced Urothelial Carcinoma. Clin Genitourin Cancer. Oct 2022;20(5):e440-e452. doi:10.1016/j.clgc.2022.06.001
Makrakis D, Talukder R, Diamantopoulos LN,… Jain J… et al. Association of prior local therapy and outcomes with programmed-death ligand-1 inhibitors in advanced urothelial cancer. BJU Int. Nov 2022;130(5):592-603. doi:10.1111/bju.15603
Lee S, Reddy Mudireddy A, Kumar Pasupula D,… Statz G, Bullis T, Evans A… et al. Novel Machine Learning Approach to Predict and Personalize Length of Stay for Patients Admitted with Syncope from the Emergency Department. J Pers Med. Dec 20 2022;13(1)doi:10.3390/jpm13010007
Kumar B, Zetumer S, Swee M, Endelman ELK, Suneja M, Davis B. Reducing Delays in Diagnosing Primary Immunodeficiency Through the Development and Implementation of a Clinical Decision Support Tool: Protocol for a Quality Improvement Project. JMIR Res Protoc. Jan 4 2022;11(1):e32635. doi:10.2196/32635
Kroll C, Zandvakili A. Delay in desmopressin therapy: Disaster in waiting. J Clin Pharm Ther. Dec 2022;47(12):2376-2378. doi:10.1111/jcpt.13807
Koshkin VS, Henderson N, James M,… Jain J… et al. Efficacy of enfortumab vedotin in advanced urothelial cancer: Analysis from the Urothelial Cancer Network to Investigate Therapeutic Experiences (UNITE) study. Cancer. Mar 15 2022;128(6):1194-1205. doi:10.1002/cncr.34057
Jónsdóttir H, Sanders ML, Goettsche L, et al. Dual diagnosis of histiocytoid Sweet syndrome and anti-neutrophil cytoplasmic antibody-associated vasculitis. JAAD Case Rep. May 2022;23:117-119. doi:10.1016/j.jdcr.2022.03.007
Hung C, Shibli-Rahhal A. Denosumab Use in Adults With Fibrous Dysplasia: Case Reports and Review of the Literature. Endocr Pract. Nov 2022;28(11):1196-1201. doi:10.1016/j.eprac.2022.07.012
Hung C, Muñoz M, Shibli-Rahhal A. Anorexia Nervosa and Osteoporosis. Calcif Tissue Int. May 2022;110(5):562-575. doi:10.1007/s00223-021-00826-3
Hung C, Mathews KD, Shibli-Rahhal A. Effect of Denosumab on Bone Health in Adult Patients with Duchenne/Becker Muscular Dystrophy: A Report of 2 Cases. JBJS Case Connect. Mar 16 2022;12(1) doi:e21.0066410.2106/jbjs.Cc.21.00664
Gutierrez WR, Scherer A, Rytlewski JD, et al. Augmenting chemotherapy with low-dose decitabine through an immune-independent mechanism. JCI Insight. 2022;7(22)doi:10.1172/jci.insight.159419
Durham K, Zhang X, Bosch DE, Ashat M. Duodenal adenocarcinoma presenting as duodenal cystic dystrophy. Gastrointest Endosc. Aug 2022;96(2):378-380. doi:10.1016/j.gie.2022.04.021
Chen BC, Chen SJT, Duchman KR, Sekar P. Extra-articular tophaceous gout of the Achilles tendon mimicking infection. BMJ Case Rep. Mar 2 2022;15(3)doi:10.1136/bcr-2021-247647
Cascio JA, Walsh M, Hoenig K, Davis B. Treatment of a 4-year-old boy with mepolizumab for lymphocytic hypereosinophilic syndrome. Ann Allergy Asthma Immunol. Aug 2022;129(2):254-255. doi:10.1016/j.anai.2022.04.031
Becker T, Smith M, Parsons M, Goto M. Non-tuberculous mycobacterial thoracic osteomyelitis in an immunocompetent host: a rare presentation of Mycobacterium kansasii. BMJ Case Rep. May 26 2022;15(5)doi:10.1136/bcr-2022-249629
Vo M, Dallaghan GB, Borges N,… Winward J… et al. Planning for Happenstance: Helping Students Optimize Unexpected Career Developments. MedEdPORTAL. Feb 8 2021;17:11087. doi:10.15766/mep_2374-8265.11087
Vather-Wu N, Krasowski MD, Mathews KD, Shibli-Rahhal A. Vitamin D Level Stability in Dystrophinopathy Patients on Vitamin D Supplementation. J Neuromuscul Dis. 2021;8(4):481-487. doi:10.3233/jnd-200625
Trivedi SP, Kopp Z, Williams PN,… Hupp D… et al. Who is Responsible for Discharge Education of Patients? A Multi-Institutional Survey of Internal Medicine Residents. J Gen Intern Med. Jun 2021;36(6):1568-1575. doi:10.1007/s11606-020-06508-4
Statz GM, Williford NN, Sardone VR, et al. A 31-Year-Old Man With Angina Pectoris Resulting From Large Vessel Vasculitis. JACC Case Rep. Aug 4 2021;3(9):1191-1193. doi:10.1016/j.jaccas.2021.04.015
Smith M, Kobayashi T, Sekar P. Antibody testing to distinguish between histoplasmosis and blastomycosis. BMJ Case Rep. May 31 2021;14(5)doi:10.1136/bcr-2021-243587
Singh A, Cole RC, Espinoza AI,… Evans A… et al. Timing variability and midfrontal ~4 Hz rhythms correlate with cognition in Parkinson's disease. NPJ Parkinsons Dis. Feb 15 2021;7(1):14. doi:10.1038/s41531-021-00158-x
Rytlewski JD, Scalora N, Garcia K, et al. Photodynamic Therapy Using Hippo Pathway Inhibitor Verteporfin: A Potential Dual Mechanistic Approach in Treatment of Soft Tissue Sarcomas. Cancers. 2021;13(4):675. doi:10.3390/cancers13040675
Rytlewski J, Milhem MM, Monga V. Turning ‘Cold’ tumors ‘Hot’: immunotherapies in sarcoma. Annals of Translational Medicine. 2021;9(12):1039-1039. doi:10.21037/atm-20-6041
Rieth JM, Swami U, Mott SL, et al. Melanoma Brain Metastases in the Era of Targeted Therapy and Checkpoint Inhibitor Therapy. Cancers. 2021;13(7):1489. doi:10.3390/cancers13071489
Rieth JM, Bowen RC, Milhem MM, Boldt HC, Binkley EM. Presumed Melanoma of Unknown Primary Origin Metastatic to the Choroid Mimics Primary Uveal Melanoma. Case Reports in Ophthalmology. 2021;12(3):987-993. doi:10.1159/000521199
Qaqish TR, Chainani A, Batchelor E,… Jonsdottir H… et al. Spontaneous bilobar torsion managed with pneumopexy. JTCVS Tech. Jun 2021;7:301-304. doi:10.1016/j.xjtc.2021.01.027
Pysick H, Dexter D, Lindsay C. Verbal Amnesia Secondary to Unilateral Infarct of the Mediodorsal Thalamic Nucleus. Wmj. Oct 2021;120(3):247-249.
Kotwal V, Mbachi C, Wang Y,… Rosenstengle C… et al. A Novel Score to Predict Esophageal Varices in Patients with Compensated Advanced Chronic Liver Disease. Digestive Diseases and Sciences. 2021;66(6):2084-2091. doi:10.1007/s10620-020-06456-3
Kobayashi T, Salinas JL, Ten Eyck P, Chen B, et al. Palliative care consultation in patients with Staphylococcus aureus bacteremia. Palliat Med. Apr 2021;35(4):785-792. doi:10.1177/0269216321999574
Khaki AR, Li A, Diamantopoulos LN,… Jain J… et al. A New Prognostic Model in Patients with Advanced Urothelial Carcinoma Treated with First-line Immune Checkpoint Inhibitors. Eur Urol Oncol. Jun 2021;4(3):464-472. doi:10.1016/j.euo.2020.12.006
Jennings B, Rieth J, Snyders T, Milhem M. Sustained response to imatinib in patient with extraskeletal myxoid chondrosarcoma and novel <i>KIT</i> mutation. BMJ Case Reports. 2021;14(8):e242039. doi:10.1136/bcr-2021-242039
Garje R, Elhag D, Yasin HA, Acharya L, Vaena D, Dahmoush L. Comprehensive review of chromophobe renal cell carcinoma. Crit Rev Oncol Hematol. Apr 2021;160:103287. doi:10.1016/j.critrevonc.2021.103287
Esagian SM, Khaki AR, Diamantopoulos LN,… Jain J… et al. Immune checkpoint inhibitors in advanced upper and lower tract urothelial carcinoma: a comparison of outcomes. BJU Int. Aug 2021;128(2):196-205. doi:10.1111/bju.15324
Chen BC, Kobayashi T, O'Rourke H, Sekar P. Staphylococcus aureus osteomyelitis causing Brodie's abscess of the tibia in an adult man. BMJ Case Rep. Jan 18 2021;14(1)doi:10.1136/bcr-2020-240836
Chen B, Kobayashi T, Samra H, Sekar P. Native joint septic arthritis due to Kingella kingae in an adult. IDCases. 2021;24:e01106. doi:10.1016/j.idcr.2021.e01106
An J, Packiam VT, Chennamadhavuni A,… Jain J… et al. Patient Characteristics and Survival Outcomes of Non-Metastatic, Non-Clear Cell Renal Cell Carcinoma. Front Oncol. 2021;11:786307. doi:10.3389/fonc.2021.786307
Abdelhamid AA, Kobayashi T, Tholany J, Sekar P. Recurrent Cutibacterium acnes prosthetic valve endocarditis. BMJ Case Rep. Jul 29 2021;14(7)doi:10.1136/bcr-2021-243878
Winward J, Lyckholm L, Brown SM, Mokadem M. Case of relapsing sulfasalazine-induced hypersensitivity syndrome upon re-exposure. BMJ Case Rep. Sep 15 2020;13(9)doi:10.1136/bcr-2020-235803
Vargas Buonfiglio LG, Vanegas Calderon OG, Cano M, et al. Seasonal Antimicrobial Activity of the Airway: Post-Hoc Analysis of a Randomized Placebo-Controlled Double-Blind Trial. Nutrients. Aug 27 2020;12(9)doi:10.3390/nu12092602
Vargas Buonfiglio LG, Comellas AP. Mechanism of ambient particulate matter and respiratory infections. J Thorac Dis. Mar 2020;12(3):134-136. doi:10.21037/jtd.2019.12.33
Struble RD, Knox BA, Richter KP, Ellerbeck EF. Insurance coverage and utilization of nicotine patches after receipt of a prescription. Subst Abus. 2020;41(3):307-310. doi:10.1080/08897077.2019.1671935
Statz GM, Olshansky B. Editorial commentary: Vagal nerve stimulation for myocardial ischemia-reperfusion injury: Hope or Hype? Trends Cardiovasc Med. Nov 2020;30(8):489-490. doi:10.1016/j.tcm.2019.12.004
Simms A, Kobayashi T, Endelman L, Sekar P. Disseminated histoplasmosis presenting as bilateral lower extremity paresis. Int J Infect Dis. Jun 2020;95:265-267. doi:10.1016/j.ijid.2020.03.072
Rieth JM, Chen SJT, Bennett DL, Suneja M. Isolated Histoplasma Tenosynovitis in a Patient on Adalimumab. Mayo Clinic Proceedings. 2020;95(6):1212. doi:10.1016/j.mayocp.2020.02.023
Ravi P, Mantia C, Su C,… Elhag D… et al. Evaluation of the Safety and Efficacy of Immunotherapy Rechallenge in Patients With Renal Cell Carcinoma. JAMA Oncol. Oct 1 2020;6(10):1606-1610. doi:10.1001/jamaoncol.2020.2169
Rasmussen TP, Bullis TC, Girotra S. Targeted Temperature Management for Treatment of Cardiac Arrest. Current Treatment Options in Cardiovascular Medicine. 2020;22(11)doi:10.1007/s11936-020-00846-6
Miller NJ, Khaki AR, Diamantopoulos LN,… Jain J… et al. Histological Subtypes and Response to PD-1/PD-L1 Blockade in Advanced Urothelial Cancer: A Retrospective Study. J Urol. Jul 2020;204(1):63-70. doi:10.1097/ju.0000000000000761
Lu R, Kassim T, Dave D, et al. Diagnostic Yield of Colonoscopy in Young Adults with Lower Gastrointestinal Symptoms in a Multicenter Midwest Cohort. Dig Dis. 2020;38(6):484-489. doi:10.1159/000506073
Khaki AR, Li A, Diamantopoulos LN,… Jain J… et al. Impact of performance status on treatment outcomes: A real-world study of advanced urothelial cancer treated with immune checkpoint inhibitors. Cancer. Mar 15 2020;126(6):1208-1216. doi:10.1002/cncr.32645
Jain J, Stein J, Garje R. Evaluation of Checkpoint Inhibitors in Cancer Patients With End-stage Renal Disease on Hemodialysis: Case Series and Review of the Literature. J Immunother. Oct 2020;43(8):244-249. doi:10.1097/cji.0000000000000327
Hoffman RM, Atallah RP, Struble RD, Badgett RG. Lung Cancer Screening with Low-Dose CT: a Meta-Analysis. J Gen Intern Med. Oct 2020;35(10):3015-3025. doi:10.1007/s11606-020-05951-7
Hammel JA, Elhag D, Ferguson NN. Subungual hemorrhage from an epidermal growth factor receptor inhibitor. Cutis. Jan 2020;105(1):E15-e16.
Gebska MA, Williford NN, Schadler AJ, et al. Pharmacological vs Exercise Stress Echocardiography for Detection of Cardiac Allograft Vasculopathy. Mayo Clin Proc Innov Qual Outcomes. Feb 2020;4(1):65-75. doi:10.1016/j.mayocpiqo.2019.09.003
Garje R, An J, Greco A, Vaddepally RK, Zakharia Y. The Future of Immunotherapy-Based Combination Therapy in Metastatic Renal Cell Carcinoma. Cancers (Basel). Jan 7 2020;12(1)doi:10.3390/cancers12010143
Feng A, Masadeh M, Murali AR. Recurrent Isolated Hyperbilirubinemia From Drug-Induced Impaired Hepatic Bilirubin Uptake. Hepatology. Sep 2020;72(3):1145-1147. doi:10.1002/hep.31154
Elkaryoni A, Altibi AM, Khan MS,… Hassan A… et al. Global longitudinal strain assessment of the left ventricle by speckle tracking echocardiography detects acute cellular rejection in orthotopic heart transplant recipients: A systematic review and meta-analysis. Echocardiography. Feb 2020;37(2):302-309. doi:10.1111/echo.14586
Chen BC, Kobayashi T, Ford B, Sekar P. Late prosthetic shoulder joint infection due to Actinomyces neuii in an adult man. BMJ Case Rep. Sep 29 2020;13(9)doi:10.1136/bcr-2020-236350
Williford NN, Mazur A, Rhodes T, Demetroulis E, Gebska MA. Coronary Spasm and Polymorphic Ventricular Tachycardia One Year After Takotsubo. Mayo Clin Proc Innov Qual Outcomes. Jun 2019;3(2):231-234. doi:10.1016/j.mayocpiqo.2019.01.001
Williford NN, Gebska MA. Natural history of Takotsubo syndrome - Arrhythmogenic dilemma. Int J Cardiol. Feb 1 2019;276:41. doi:10.1016/j.ijcard.2018.11.014
Williford NN, Chapleau MW, Olshansky B. Neurohormones in Vasovagal Syncope: Are They Important? J Am Heart Assoc. Jun 18 2019;8(12):e013129. doi:10.1161/jaha.119.013129
Rasmussen TP, Williford NN, DeZorzi C,… Boyle B… et al. Women Hospitalized for Acute on Chronic Decompensated Systolic Heart Failure Receive Less Furosemide Compared to Men. Cardiol Res Pract. 2019;2019:1505142. doi:10.1155/2019/1505142
Masadeh M, Dave D, El Abiad R. Endoscopic Ultrasound Guidance in Diagnosing a Rare Case of Lung Adenocarcinoma Metastatic to the Pancreas. Pancreas. Apr 2019;48(4):e30-e31. doi:10.1097/mpa.0000000000001285
Laderian B, Koehn K, Holman C, Lyckholm L, Furqan M. Association of Hemophagocytic Lymphohistiocytosis and Programmed Death 1 Checkpoint Inhibitors. J Thorac Oncol. Apr 2019;14(4):e77-e78. doi:10.1016/j.jtho.2018.11.035
Koval OM, Nguyen EK, Santhana V, et al. Loss of MCU prevents mitochondrial fusion in G(1)-S phase and blocks cell cycle progression and proliferation. Sci Signal. Apr 30 2019;12(579)doi:10.1126/scisignal.aav1439
Klein M, Khan M, Salinas JL, Sanchez R. Disseminated pulmonary histoplasmosis in immunocompetent patients: a common epidemiological exposure. BMJ Case Rep. Mar 20 2019;12(3)doi:10.1136/bcr-2018-227994
Grumbach IM, Nguyen EK. Metabolic Stress. Arterioscler Thromb Vasc Biol. Jun 2019;39(6):991-997. doi:10.1161/atvbaha.118.312196
Greco A, Safi D, Swami U, Ginader T, Milhem M, Zakharia Y. Efficacy and Adverse Events in Metastatic Melanoma Patients Treated with Combination BRAF Plus MEK Inhibitors Versus BRAF Inhibitors: A Systematic Review. Cancers (Basel). Dec 5 2019;11(12)doi:10.3390/cancers11121950
DeZorzi C, Boyle B, Qazi A, et al. Administrative Billing Codes for Identifying Patients With Cardiac Arrest. J Am Coll Cardiol. Apr 2 2019;73(12):1598-1600. doi:10.1016/j.jacc.2019.01.030
Ansari MS, Tanaka T, Laroia ST, Sun S. Feasibility of Hepatology-Directed Microwave Ablation in Management of Hepatocellular Carcinoma in North America: A Pilot Project. Ann Hepatol. Jan-Feb 2019;18(1):11-13. doi:10.5604/01.3001.0012.7855
Williford NN, Ward CC, Olshansky B. Evaluation and Management of Syncope: Comparing the Guidelines of the American College of Cardiology/American Heart Association/Heart Rhythm Society and the European Society of Cardiology. J Innov Card Rhythm Manag. Dec 2018;9(12):3457-3463. doi:10.19102/icrm.2018.091208
Willey J, Mentias A, Vaughan-Sarrazin M, McCoy K, Rosenthal G, Girotra S. Epidemiology of lower extremity peripheral artery disease in veterans. J Vasc Surg. Aug 2018;68(2):527-535.e5. doi:10.1016/j.jvs.2017.11.083
Vargas Buonfiglio LG, Borcherding JA, Frommelt M,… Duchman B… et al. Airway surface liquid from smokers promotes bacterial growth and biofilm formation via iron-lactoferrin imbalance. Respir Res. Mar 10 2018;19(1):42. doi:10.1186/s12931-018-0743-x
O'Malley Y, Rotti PG, Thornell IM,… Durham K… et al. Development of a polarized pancreatic ductular cell epithelium for physiological studies. J Appl Physiol (1985). Jul 1 2018;125(1):97-106. doi:10.1152/japplphysiol.00043.2018
Nguyen EK, Koval OM, Noble P, et al. CaMKII (Ca(2+)/Calmodulin-Dependent Kinase II) in Mitochondria of Smooth Muscle Cells Controls Mitochondrial Mobility, Migration, and Neointima Formation. Arterioscler Thromb Vasc Biol. Jun 2018;38(6):1333-1345. doi:10.1161/atvbaha.118.310951
Mohsen A, Alqasrawi M, Shantha GPS, DeZorzi C, Panaich S. Comparison of Radial Artery Occlusion Following Transradial Access for Percutaneous Coronary Intervention Using Sheath-based versus Sheathless Technique. Sci Rep. Aug 13 2018;8(1):12026. doi:10.1038/s41598-018-30462-1
Garje R, An JJ, Sanchez K, Greco A, et al. Current Landscape and the Potential Role of Hypoxia-Inducible Factors and Selenium in Clear Cell Renal Cell Carcinoma Treatment. Int J Mol Sci. Dec 1 2018;19(12)doi:10.3390/ijms19123834
Elhag D, Dexter F, Elhakim M, Epstein RH. Many US hospital-affiliated freestanding ambulatory surgery centers are located on hospital campuses, relevant to interpretation of studies involving ambulatory surgery. J Clin Anesth. Sep 2018;49:88-91. doi:10.1016/j.jclinane.2018.06.021
DeZorzi C, Harris KI. Secret Sarcoma: A Cardiac Mass Disguised as Influenza. Case Rep Cardiol. 2018;2018:8628365. doi:10.1155/2018/8628365
DeZorzi C, Fernandez-Ruiz R, Gupta S, Harris K. Cerebral amyloid angiopathy mimicking central nervous system metastases: a case report. J Med Case Rep. May 14 2018;12(1):133. doi:10.1186/s13256-018-1655-6
DeZorzi C. Radiation-Induced Coronary Artery Disease and Its Treatment: A Quick Review of Current Evidence. Cardiol Res Pract. 2018;2018:8367268. doi:10.1155/2018/8367268
Research Elective
The research elective is a 2- or 4-week block where residents are provided dedicated time to pursue their scholarly interests. Residents work with a mentor that the resident chooses. This mentor helps to provide guidance on how to be most efficient with this dedicated research time. This block is available during resident’s second and/or third year.
StARR Program
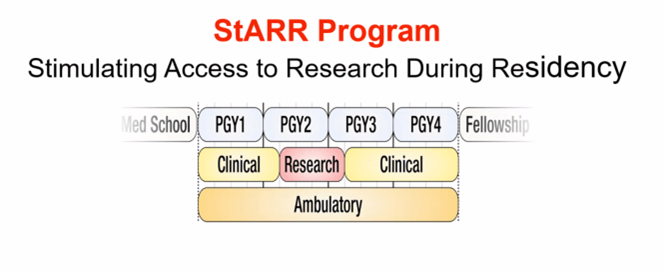 The Stimulating Access to Research during Residency (StARR) program is a 1-year opportunity dedicated to immersing residents in a research experience. This program is only 1 of approximately 10 programs offered as a part of internal medicine residency nationally. It is funded by a $1.3M R38 grant funded by the NIH’s National Heart, Lung, and Blood Institute (NHLBI). Residents will work directly with a research mentor for the entirety of the StARR year (and beyond).
The Stimulating Access to Research during Residency (StARR) program is a 1-year opportunity dedicated to immersing residents in a research experience. This program is only 1 of approximately 10 programs offered as a part of internal medicine residency nationally. It is funded by a $1.3M R38 grant funded by the NIH’s National Heart, Lung, and Blood Institute (NHLBI). Residents will work directly with a research mentor for the entirety of the StARR year (and beyond).
Graduates of the StARR program are also eligible to apply for K38 grants while in fellowship.
Contact information:

David Stoltz, MD, PhD
Director, StARR Program
david-stoltz@uiowa.edu
Physician Scientist Training Pathway
The Physician-Scientist Training Pathway (PSTP) is designed to streamline postgraduate training and to foster early career development of physician-scientists who will be future leaders in academic medicine. The PSTP integrates residency training, clinical fellowship, and postdoctoral research training. We support research training with numerous T32 training grants and offer a large breath of clinical program. Residents who are selected for the PSTP are guaranteed a subspecialty fellowship position and can complete residency training in two years. They are also eligible for an additional academic allowance and supplemental salary during the research phase of their training.
The PSTP is available to applicants who have completed a Medical Scientist Training Program (MSTP).
Contact Information
Marian Carson
PSTP Program Coordinator
200 CMAB
Iowa City, IA 52242
(319) 335-6760
marian-carson@uiowa.edu
David Stoltz, MD, PhD
Director, PSTP Program
david-stoltz@uiowa.edu
Mentorship at Iowa
At Iowa, we recognize the importance of quality mentorship in helping our residents lay the foundation for personal and professional success in their future careers. We, as the residency administration, will do as much as we possibly can to help match our residents with mentors that can help them grow. Our distinction tracks (links), pathways (link), StARR program (link), and PSTP (link) all provide formal avenues of identify mentors and working with them towards a specific goal.
Additionally, research leaders from across the subspecialties of internal medicine talk to the residents at noon conference on an annual basis about the research mentors in their department who have active research projects that are looking for help from residents. Furthermore, one of our Associate Program Directors’ role in the residency program is dedicated to facilitating mentorship, scholarly activity, and application to fellowship. They are our go-to person to help find mentorship for our residents’ unique scholarly interests.
Since switching the X+Y schedule, we have also found that residents now have the opportunity to have a longitudinal clinical experience with a faculty in a subspecialty of their interest. These clinical experiences often lead to mentorship opportunities.
Beyond Residency
At Iowa, our goal is to help you achieve whatever career goal you envision for yourself by providing you the opportunities and experiences you need to take the next step in your career path. We have a mentorship system, flexibility in rotation, pathways, and distinction tracks that can all be tailored to help you get the experiences you need to be prepared to excel in the next step of your career journey.
From 2018-2023, 70% of our residents have gone on to pursue fellowship immediately after residency. Many of our residents match in to fellowship is Iowa, which speaks to the collegial education environment that extends beyond the internal medicine residency to the whole department of internal medicine. We have also had great success matching residents into fellowships across the country. (see map below)
While the majority of our residents go on to fellowship, the focus of our residency is on training our residents to be fantastic internists. From From 2018-2023, approximately 28% of our residents have gone on to practice primary care or hospital medicine after residency, and they have accepted jobs all across the country.
Additionally, we have had two residents go on to study health informatics and one pursue a post-graduate research position (T32 grant).
Destinations of 2024 Graduates
Fellowship Training Institutions (2020-2025)
|
|
|
Where Are They Now?
Read about where some of our program graduates have landed in our Where Are They Now series!
Check back often for additional profiles.
Resident Life and Well-being

At the University of Iowa Internal Medicine Program, we know that we can only achieve our mission of helping our residence excel as clinicians, educators, and scholars in a culture that emphasizes collaboration and belonging and promotes wellness.
Our culture wasn’t built overnight and it takes work to maintain. But we are proud of the way our program runs and the way we all work together as a team. Our culture isn’t something that just stays in the hospital either. We are proud of how our residents spend time with each other both in and out of the hospital.
Here is what we do to maintain our inclusive culture and promote wellness:
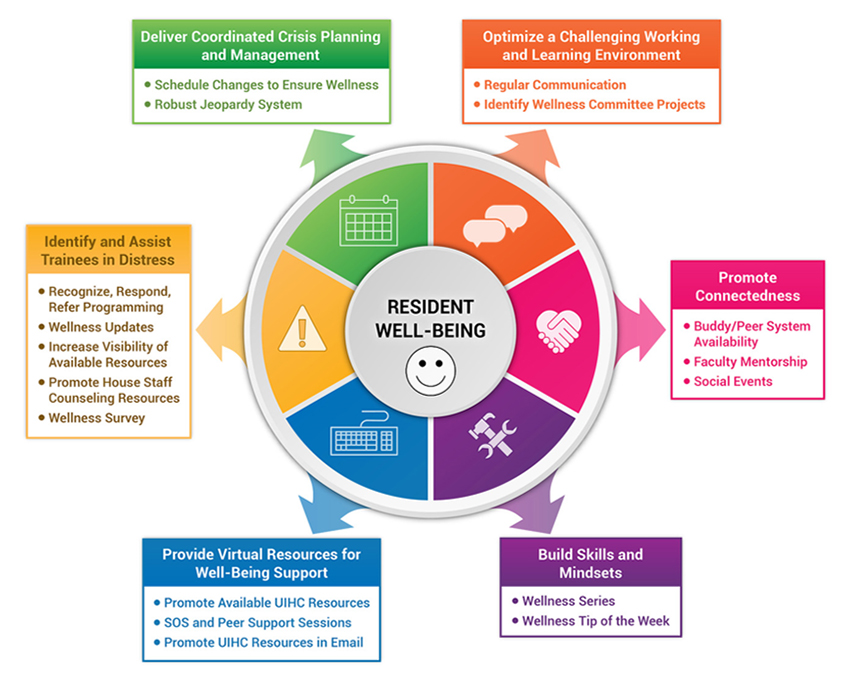
Transition to Residency
The transition to residency can be a tough time. Many of our residents are moving to Iowa City for the first time. We make sure that our residents feel right at home as soon as possible with a robust orientation and a peer mentoring program that connects residents in order to facilitate inclusion from day 1.
Peer Mentoring program
Each incoming intern is paired with a senior resident prior to orientation. The mentor match is based on several factors including hobbies and career interests. As interns arrive to Iowa City, they are encouraged to meet with their mentors. Mentors are available for any concerns that come up at any point in time throughout the year. Mentors are happy to answer questions about housing, adjustment challenges, and resident life in general. Over time, peer mentors become close colleagues who interns can rely on in and outside of the hospital.
Orientation focused on Strategies for Success
During orientation, the new interns get to know the chief residents, who will be the go-to people for any concern or question throughout the year. The chief residents go over practical skills like how to hand-off patients to the night team, how to stay organized on the wards, how to use the University of Iowa’s online resources, and how to perform the common procedures in internal medicine, like central venous catheter placement, paracentesis, thoracentesis, and lumbar puncture.
Resident-to-Resident Epic Training
In 2021, residents initiated a resident-to-resident epic training in place of the generic epic training. Residents teach practical skills and share SmartPhrases that help the interns hit the ground running on day one.
New resident Objective Structured Clinical Experience (OSCE)
During orientation, our residents participate in an Objective Structured Clinical Experience (OSCE). The goal of this OSCE is to get interns back in the swing of seeing patients again and also gives us an opportunity to provide just-in-time feedback to residents on skills to develop even prior to their first experience on the wards.
We were one of the first programs to implement an OSCE during orientation and our pioneering work on the OSCE (Assessing Entrustable Professional Activities Using an Orientation OSCE: Identifying the Gaps - PubMed (nih.gov)) was cited by the ACGME when it recommended all US resident programs adopt this evaluation tool during orientation.
Learn more about our past OSCE sessions: Seven years, seven OSCEs
Connection Between Peers
We have an amazing community of residents who enjoy spending time with each other both in and out of the hospital. On the long days (and there will be long days) and your senior resident stays late too just to help you get your work done, that’s what we are about here at Iowa.
Welcome Picnic during Orientation
As a way to help interns get to know those associated with the residency program, a welcome gathering is held during orientation for residents, faculty, and their family.
Annual Resident Retreat
Each year, a 1-day off-campus workshop for each residency class is organized to provide further skill development in areas of communication, teaching, leadership, team-building, and self-development. On the day of the workshop, all of the residents’ hospital responsibilities are covered by the other cohorts, which provides a great environment for residents to relax and have fun together.



Y-week supper clubs
One of the great benefits of having an X+Y schedule is that there is a cohort of residents that all regularly have the same weekend off the whole three years of residency. These cohorts often go to a local restaurant together after the academic half-day on Thursday.


Humanities and Wellness Committee Activities
Throughout the year, the Humanities and Wellness Committee organizes various social activities throughout the year. These include a trip to the local apple orchard and renting out the local independent movie theater for the showing of a movie!
GME House Staff Council Activities
The GME House Staff Council organizes multiple events for all residents at UIHC throughout the year. Last year, these events included going to two Iowa women’s basketball game (who played in the NCAA National Championship game last season.
Food truck Thursdays
During the warmer months, the entire scientific community at the University of Iowa is invited to relax around the lunch hour on Thursday. Food trucks come from across the state and park just outside the hospital. There is live music onsite as well.
Winter Recognition Event
The Internal Medicine Residency hosts an annual winter gathering at a local restaurant to recognize the hard work and dedication of our residents. It is a welcome time to relax and enjoy tme away from the hospital with friends and colleagues.



Resident Graduation House Staff dinner
In June, the department hosts a farewell dinner program honoring the graduating residents and celebrating their accomplishments.
Resident hangouts throughout the year
Our residents are great about having each other over just to hang out and have fun outside the hospital. These activities facilitated by the easy navigability of the city, the proximity of downtown Iowa City, and the many parks and outdoor activities nearby.
There are also many interest groups that are available to our residents as part of the University community. These include the UIHC Writers’ Group, the Internal Medicine Book Club, and faculty/staff orchestra to name a few examples.




Resident Lounge
The Internal Medicine Resident Lounge is a community gathering space equipped with a small kitchen, a treadmill workstation, and many computers. Residents often work from this space when on consult rotations.
Supporting Healthy Lifestyles
During your residency at Iowa, we will make sure that you have access to the resources you need to practice the habits of healthy living in your everyday life.
Employee Assistance Program
Free and confidential counseling services designed for employees to assist with emotional health, stress, fatigue, depression, suicide prevention, grief, and substance use.
There is a phone line that is answered 24/7 in case of immediate assistance.
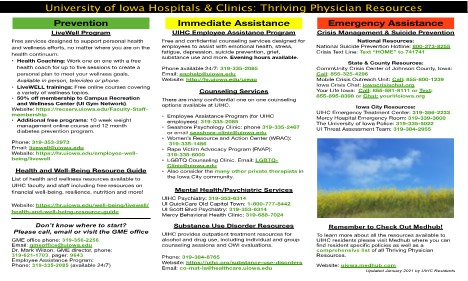
Resident Workout facility
There is a work-out facility with showers in the hospital that residents have access to 24/7. This facility is operated by the Office of Graduate Medical Education.
LiveWell Program
A gym membership that gets you access to all University gyms costs $40/month and if you go 4 times per month, the cost goes down to $20/month!
Personal health coaching is also available through this program to help great a personal plan to meet your wellness goals.
For more information, go to https://hr.uiowa.edu/employee-well-being/livewell
Opt-out medical appointments
Started during the 2023-2024 academic year, the Office of Graduate Medical Education works on setting up residents with a Primary Care Provider in a department that they are not affiliated with (for Internal Medicine, that is family medicine). Our residency program will facilitate you getting to your medical appointments, regardless of what rotation you are on.
Wellness Curriculum
For more information, go to Wellness Curriculum.
After-hours Rides
There are multiple transportation optins that will take you directly to your car if you are getting done late. These options include:
- Late Evening Staff Shuttle
- CAMBUS On-Demand Shuttle (https://transportation.uiowa.edu/cambus/routes/cambus-demand-shuttle-service)
- Nite Ride (https://niteride.its.uiowa.edu/request/#/hours)
- For more information, visit https://transportation.uiowa.edu/nighttime-transportation
GME will also pay for you to take a cab all the way home if you are too tired to drive. For more information, contact the Graduate Medical Education (GME) Office (gmeoffice@uiowa.edu)
Life in Iowa City
Iowa City is a vibrant community and a fantastic place to live during your residency. The Internal Medicine Residents have put together a list of their favorite spots in the Iowa City area. We also invite you to check out more information on Iowa City in the below links to learn more about Iowa City.
Why Iowa
Innovations
Teaching Skills Curriculum
In addition to a three-year, rolling curriculum, our program also offers a dedicated teaching rotation in the third year, as well as more advanced training.
Ultrasound Curriculum
Our longitudinal training in point-of-care ultrasound (POCUS) results in residency graduates with skills that would normally only be obtained in radiology or emergency medicine programs.
Quality & Safety Curriculum
Quality improvement benefits our patients and our systems, but it also provides our residents with an opportunity to lead a focused project often resulting in a publication or presentation at a regional or national society meeting. We have carved-out protected time for this work and our VA-funded Chief Resident for Quality & Safety is just one of the mentors guiding residents.
qUIkCoach
Through the department, we have been able to develop an app available for our residents called qUIkcoach. This is a new app that is able to request and provide just-in-time feedback on a variety of different skills including clinical reasoning, communication, oral presentation, and notes. This allows for more directed feedback with a quicker turnaround time.
Ultrasound Curriculum
Point of Care Ultrasound Curriculum Overview
The University of Iowa Internal Medicine Residency Program Point-of-Care Ultrasound (POCUS) Curriculum is a longitudinal, integrated, and progressive learning experience. The POCUS curriculum is focused on teaching basic bedside ultrasonography and how it is utilized and applied to patient care in clinical internal medicine. The curriculum is integrated into and taught longitudinally during the academic half day during each resident’s ambulatory week (y-week). POCUS instruction is delivered by experienced faculty members, critical care fellows, and chief residents. POCUS skills assessments are completed for residents during each year of their training and the POCUS curriculum is modified on a yearly basis to best adapt to the needs of the trainees.
Curriculum Goal: At the end of the longitudinal POCUS curriculum, the resident will be able to acquire, interpret, and apply focused cardiac, lung, pleural, abdominal, and vascular ultrasound imaging into their clinical reasoning and medical decision making.
Teaching Methods:
- Independent pre-workshop learning materials (POCUS textbook chapters, online modules, etc)
- Short didactic sessions
- Hands-on scanning of simulated patients with live faculty mentors and real-time feedback
- Pathological image interpretation sessions
- Interactive ultrasound case studies
Modules:
| Basic POCUS Modules (PGY-1) | Advanced POCUS Modules (PGY-2 and above) |
|
|
Assessment: Pre- and post-curriculum assessment is completed annually to assess each individual trainee’s skills and knowledge acquisition and retention. These yearly assessments are also used to assess the curriculum and guide ongoing improvements in the POCUS curriculum. Assessment is completed using live ultrasound skills testing with faculty proctors, an electronic ultrasound knowledge assessment, and a resident survey.

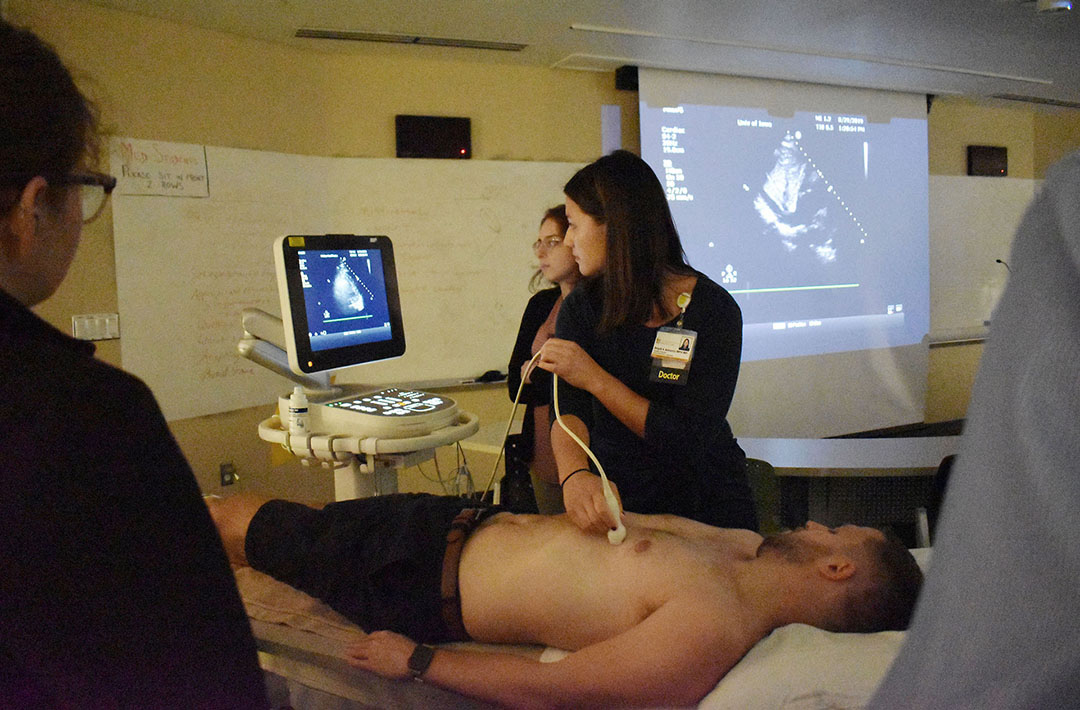
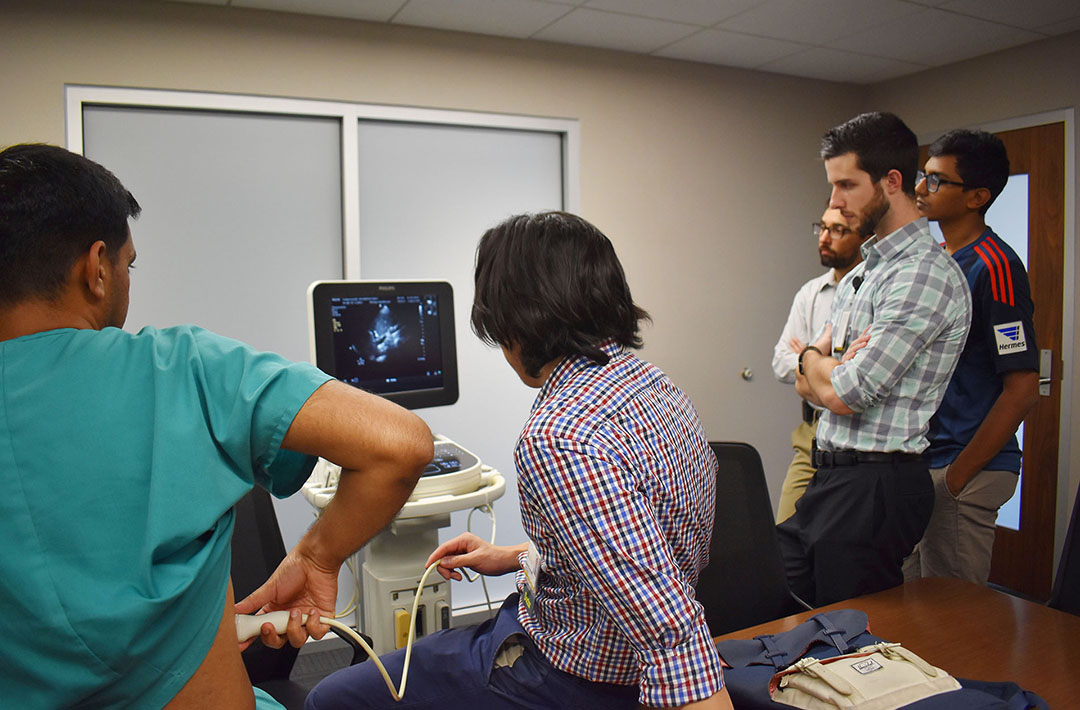

Quality Improvement Curriculum
![]()
Check out the
QI information on our blog
Resident Quality Improvement Curriculum
The Internal Medicine Residency Program at the University of Iowa is committed to engaging residents in team-based Patient Safety/Quality Improvement projects to develop their knowledge and skills. It is our goal for every resident to be empowered to impact the quality and safety of their patients’ care during their residency and in their future careers. Our ground breaking curriculum was published in the Journal of Graduate Medical Education.
Objectives
- Actively and meaningfully participate in a team quality improvement project
- Work effectively with inter-professional teams on continuous quality improvement
- Apply continuous quality improvement to patient care
- Disseminate work in scholarly format
- Make a difference in the safety and quality of care of our current and future patients
Meet our Quality Improvement Leaders

Carly Kuehn, MD
Educational Director - Safety and Quality
Clinical Professor of Internal Medicine

Samuel Zetumer, MD
Chief Resident of Quality and Safety
Iowa City VA Medical Center
Quality Improvement Scholarship
The University of Iowa Department of Medicine understands that Quality Improvement and Patient Safety presents a phenomenal opportunity for scholarship for our residents. To showcase our commitment to our patient’s safety and to provide an avenue for scholarship the University of Iowa Hospitals and Clinics host an annual Quality and Safety Symposium in which our resident teams are given the opportunity, encouragement, resources, and mentorship to submit and present their projects. After this, many teams submit their projects to large regional and national meetings.
Since the development of our curriculum we have had…
- 50+ resident led QI Projects
- 30+ resident led QI Projects presented at our local Quality and Safety Symposium
- 25 resident teams present oral presentations or posters at SGIM Midwest Regional Meeting
- 7 resident teams present posters at SGIM National Meeting
- 2 resident teams present at Medicine or Psychiatry Conferences
Resident Quotes
“I felt as though I was making a quality change to improve the outpatient experience.”
“The QI curriculum gave us an opportunity for ownership over real positive change for our patients.”
“I actually know now the basics of how to design, implement, and interpret the results of a quality improvement project, which I didn’t know before.”
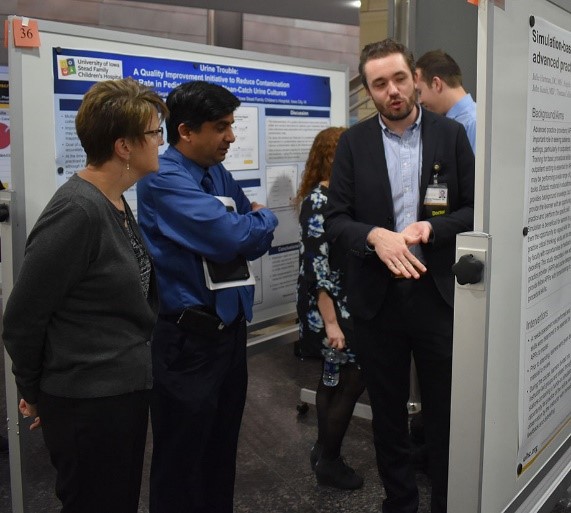
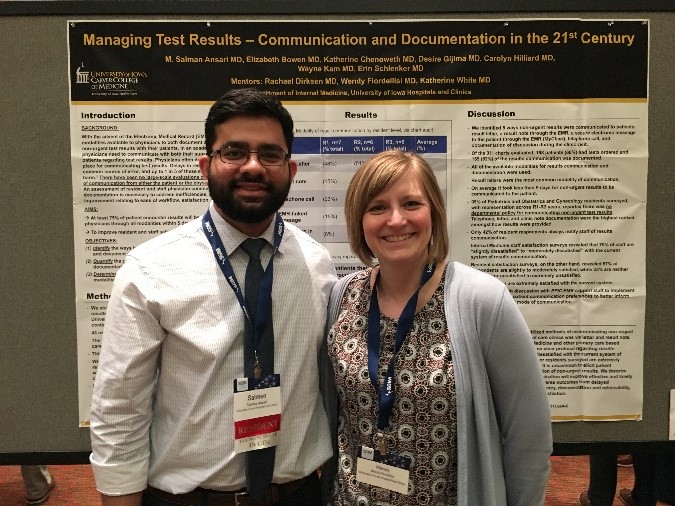
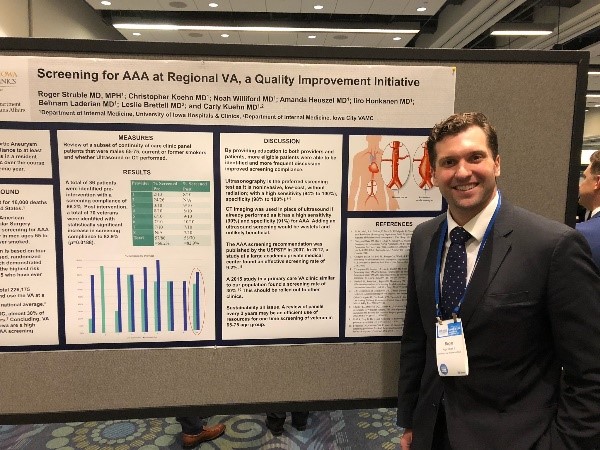
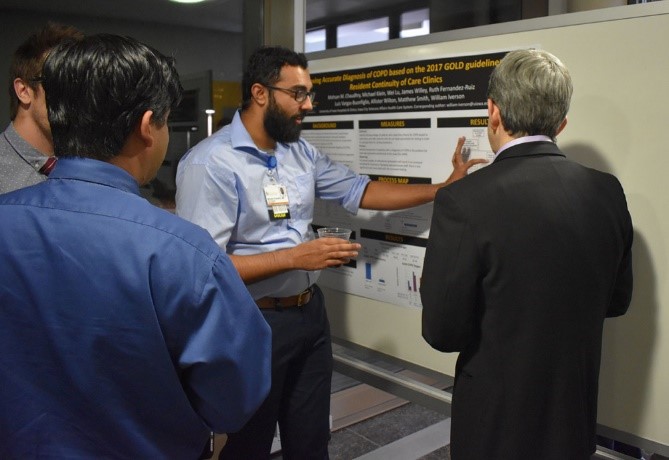
Individualization
We are committed to tailoring our residents experience at Iowa to their career goals. Here is how we do that:
How We Improve
We are committed to being a program that is continually improving. That requires a lot of resident input. He are the formal ways we get that input.
House Staff
One per month, residents and residency leadership gather during noon conference to talk about updates within the program and celebrate the successes of our residents. This time is also used as an open floor forum for residents to bring up concerns and provide input on changes that will help improve the residency program.
Resident Liaison Committee
The Resident Liaison Committee (RLC) is comprised of 15-18 residents that serve as representative for the entire cohort of residents. The committee provides a forum for residents to voice concerns directly with program administration and participate in the ongoing evolution of the residency program and curriculum.
Program Evaluation Committee
The Program Evaluation Committee (PEC) is charged with ensuring the quality of the residency program by overseeing program evaluation, design, and improvement.
Humanities and Wellness Committee
The Humanities and Wellness Committee (HWC) is comprised of residents in differest stages of the program, one chief resident, and one faculty. The goal of the committee is to establish a formal framework by which to improve wellness, cohesion between residents, and the residency program. The committee aims to facilitate team-building by way of mentorship and wellness events.
Recent Changes
Geo-localization of the general medicine team to the floor where all the team rooms are.
Free medical clinic now counts as a COC half day
Distinction Tracks
Increased simulation of RRTs and Codes
Restarting international health rotations
Health equities curriculum
Wellness curriculum
Framework Fridays
Master Clinician Mystery Case Series
Our People

Internal Medicine Residency Program 2022
Our faculty members make up the largest department at UI Health Care. We are a department rich in tradition and long on talent in our important mission of teaching, caring, and discovering new understandings in medicine. As teachers and mentors, our goal is to bring out your best as a physician.
Your fellow residents are, just like you, dedicated to rewarding and meaningful careers in the practice of medicine. They come to Iowa from around the world, drawn here by a comprehensive training program, outstanding work environment, and the prospect of practice opportunities and further training afforded by their experiences here.
Our patients are also part of the training equation. They come to University of Iowa Health Care to receive the very best care from experts who are passionate about delivering it in a personable way. As Iowa’s only academic medical center, we see a comprehensive mix of challenging cases and have the privilege to work with many cultures and languages.
Chief Residents
 Rachel Anderson, MD
Rachel Anderson, MD
University of Minnesota
rachel-l-anderson@uiowa.edu
My passion for internal medicine ignited during Morning Report in my third year of medical school. Watching the Chief Residents expertly guide a diverse group of learners, from first-time medical students to seasoned third-year residents preparing for fellowships, was truly inspiring. The process of clinical reasoning, from initial workup to final diagnosis, captivated me. To advance my own skills, I immersed myself in podcasts and diagnostic dilemma cases. I find great joy in discussing clinical cases and challenging my own thinking, and I look forward to a career in medical education where I can share this passion with others while continuing to learn and grow in the field of medicine.
The University of Iowa was the last program I interviewed at for residency, and it immediately felt like home. During my interview, Dr. Andy Bryant spoke passionately about resident education and shared his favorite spots to walk his dogs. Dr. Manish Suneja’s warmth and genuine interest during our virtual interview made me feel welcomed and valued. These interactions have only grown more meaningful throughout my residency.
Growing up in Northern Minnesota, I am one of the few who can claim that Iowa’s weather is significantly warmer than what I was used to. However, it is the people who truly make this program special. The incredible support, care, and clinical training I’ve experienced over the past three years have been invaluable. Serving as Chief Resident is an honor, allowing me to continue fostering the culture of excellence and support that defines our program.
Outside of work, you can find me hiking or running with my dog, Nala, or exploring local restaurants in search of the best fries in Iowa City. After my Chief year, I plan to pursue a fellowship in pulmonary and critical care medicine and a career as a clinician educator.
 Marie Finkbeiner, MD
Marie Finkbeiner, MD
University of Washington
marie-finkbeiner@uiowa.edu
I remember coming to Iowa City for the first time a few days before my intern orientation started. It was humid and overcast, very different than the dry heat of the Idaho summers I had grown up with.
The transition to a new place felt all too familiar. I had spent the last 2 years moving every 4 to 6 weeks for rotations in medical school at the University of Washington, a practice we lovingly described as “safari-ing.” Through this, I had the opportunity to see healthcare through many difference lenses—emergency medicine in Anchorage to rural full spectrum family medicine in Eastern Washington. But coming to Iowa felt different, like I was finally settling down.
Going through medical school, I had imagined what interviewing for residency would look like. I pictured myself in a nice suit, traveling around the country, touring hospitals and shaking hands with program directors as I nervously tried to find a program where I belonged. The world had other plans and instead I found myself sitting in front of my computer trying to connect (literally and metaphorically) with people across the country.
Part of why I wanted to be a Chief Resident was because of my interaction with people from this program on that interview day. The warmth, kindness, and genuineness of their character created an environment I felt safe to grow into the physician I wanted to become. Throughout my 3 years training here, this has held steadfast. Whether it be on the wards or in didactics, I’ve always been met with a nurturing hand to guide me in my growth as a person and doctor.
Over the three years I trained here, I have seen firsthand how the program bends and molds to best suit the needs and wants of the residents that occupy it. My goal as recruitment chief is to help create an environment where residents and the program can grow together, opening up an inviting space for new physicians who will join our family in the coming recruitment year. I intend to accomplish this by promoting transparency within the residency, actively listening to resident ideas and concerns and being open to creative solutions.
 Luke Morrey, MD
Luke Morrey, MD
University of Minnesota
luke-morrey@uiowa.edu
Growing up in Rochester, MN, a community renowned for its medical excellence, instilled in me a profound respect for the field of medicine. I pursued my undergraduate studies in biochemistry at Saint John’s University in central Minnesota, where my fascination with the complexity of human physiology grew stronger, guiding me toward a career in medicine.
My decision to specialize in internal medicine was solidified during my clerkship rotation at the University of Minnesota Medical School. It was there that I encountered many inspirational chief residents whose clinical skills and dedication to teaching left a mark on me. I was drawn to the University of Iowa during the first-ever round of virtual interviews for residents. I knew the program’s culture was the perfect fit for me.
During my residency at the University of Iowa, I have been fortunate to see many outstanding previous chief residents who have continually demonstrated the importance of enhancing the educational mission of our program. Their mentorship and leadership has prepared me for this role. As Chief Resident, I am committed to continuing our new simulation curriculum, which provides residents with hands-on, practical experience in a controlled environment. Additionally, I plan to further develop our didactic curriculum that emphasizes clinical reasoning, equipping residents with the critical thinking skills necessary for effective patient care. Looking ahead, I am excited about pursuing a fellowship in pulmonary and critical care, with a long-term goal of a career in academic medicine.
Outside of my professional life, I am dedicated to training as an amateur competitive power lifter, a pursuit that teaches me discipline, resilience, and smart goal-setting. I don’t do any cardio, but I chase my two-year-old around the park too, so I think that counts. He is a constant source of joy and motivation. Balancing my personal and professional responsibilities has enriched my life and provided me with a well-rounded perspective that I bring to my role as Chief Resident. I look forward to leading our excellent internal medicine residents.
 Lauren Zabel, MD
Lauren Zabel, MD
University of Kansas
lauren-zabel@uiowa.edu
I’ve lived in the Midwest my whole life, but that wasn’t necessarily the plan. I grew up in Lawrence, Kansas, and attended medical school at the University of Kansas in Kansas City. When it came time to apply for residency, I was set on leaving the Midwest. I was encouraged by mentors to apply to Iowa, but it wasn’t on my radar until interview day. After my interview I remember closing my laptop and thinking “this is my program,” and It’s been one of the best decisions I’ve ever made.
These past three years of residency have challenged me academically, professionally, and personally, but they’ve also been the best three years of my adult life. I’ve had the fortune of training in a program surrounded by leadership, staff, and colleagues that have supported me from day one and treated me like family. I’ve formed some of the best and closest friendships that I know will be lifelong. I’ve been a part of countless shenanigans with my “Y-week crew” (co-residents on the same clinic rotation schedule) including laser tag, ice skating, pumpkin carving, hatchet throwing, chicken catching, and much more.
I applied to be Chief Resident because I wanted to be a part of a program that has done so much for me. During my year as Chief Resident in Quality and Safety (CRQS), I want to promote resident involvement and education in quality improvement and patient safety, so residents will be better prepared to face these issues as a graduate. I also hope to promote our growing palliative care and Distinction in Health Equity (DIHE) education curricula. At the end of my chief year, I plan to complete additional training in palliative care fellowship.
1st Year Class

Noor-Us-Sabah Ahmad, MD
King Edward Medical University
Prelim-Ophthalmology

Aiah Alatoum, MBBS
Yarmouk University
Prelim

Mohad Awan, MD, MPH
University of Iowa

Greta Becker, MD
University of Iowa
PSTP

Madison Bellamy, MD
University of Missouri - Columbia

Zack Bracken, MD
Medical College of Wisconsin

Hailey Briseno, MD
University of Washington
(Medicine-Psychiatry)

Mahmoud Dibas, MBBS
Sulaiman Alrajhi College of Medicine
(Neurology)

Paolo Disano, MD
California Northstate University

Emily Entz, MD
University of Washington

James Eyer, MD
Meharry Medical College
(Neurology)

Kirsten Fiestan, MD
University of Michigan

Ella Gehrke, MD
University of Iowa
Prelim - Ophthalmology

Sahand Golestan, MD
Chicago Medical School at Rosalind Franklin University
(Neurology)

Halimah Hamidu-Egiebor, MD
Central Michigan University
(Medicine-Psychiatry)

Jacob Heath, MD
Brown University

Nic Heckenlaible, MD
Johns Hopkins University
Prelim - Ophthalmology

Trevor Hoggan, MD
University of Utah

Matthew Horner, MD
University of Kansas

Jennifer Houser, MD
Southern Illinois University

Shane Hursh, MD
University of Kansas School of Medicine
(Neurology)

Amanda Janquart, MD
Medical College of Wisconsin
(Neurology)

Karen Johns, MD
Albany Medical College

Trey Krupp, MD
University of Iowa

Aubri Larson, MD
Medical College of Wisconsin

Eleazar Luevano, MD
University of Oklahoma - Tulsa

Kyle Luo, MD
University of Kentucky

Caitlin Mechtly, MD
Washington State University Elson S. Floyd College of Medicine

Thomas Meram, MD
Oakland University William Beaumont School of Medicine
Prelim - Ophthalmology

Michael Miller, MD
University of Missouri - Columbia

Anika Mittal, MD
University of Missouri - Kansas City

Stacy Moroz, MD
Medical College of Wisconsin
Prelim

Michaela Norbury, MD
University of Kansas School of Medicine-Wichita
(Neurology)

Grant Ozaki, MD
University of Nebraska

Tim Porsche, MD
Indiana University School of Medicine
(Neurology)

Zoe Ryan, MD
University of Minnesota

Peter Sanchez
University of Iowa
Prelim - Ophthalmology

Trevor Simmons, MD
University of Illinois College of Medicine
(Neurology)

Juno Sung, MD
University of Iowa

Lauren Tomlinson, MD
Albany Medical College
Prelim - Ophthalmology

Patrick Vosters, MD
Medical College of Wisconsin
2nd Year Class

Joe Berei, MD
University of Illinois – Rockford

Calie Brownlee, MD
University of Arkansas

Cameron Brownlee, MD
University of Arkansas

Stefano Byer, MD, MS
University of Kansas

San Chandra, MD
University of South Dakota

Amanda Chang, MD
University of Iowa

Nick Coffey, MD, MS
University of Kentucky – Bowling Green
(Medicine-Psychiatry)
Katrina Dovalovsky, MD
University of Illinois – Rockford

Usamah ElBakkush, MD
University of Washington

Alex Greiner, MD, PhD
University of Iowa
PSTP

Mash Haque, MD
Saint Louis University

Casey Hardin, MD
University of Nebraska

Cole Howie, MD
University of Arkansas

Alp Kahveci, MD
University of Missouri – Columbia

Rachel Lee, MD
Chicago Medical School at Rosalind Franklin University

Austin Mallory, MD, MS
University of Colorado

Urvashi Mathur, MD
University of Texas – Rio Grande Valley

Dylan Miks, MD
Eastern Virginia Medical School

Megan Napier, MD
University of Washington
(Medicine-Psychiatry)

Pranav Puri, MD
Mayo Clinic Alix School of Medicine - Arizona

Maluki Radford, MD
University of Kansas – Wichita

Rob Schoeneich, MD
Chicago Medical School at Rosalind Franklin University

Trisha Slehria, MD
University of North Carolina – Chapel Hill

Carlie Sorensen, MD
University of Washington

Katrina Soyangco, MD
University of Illinois – Rockford

Quinn Vatland, MD
University of Wisconsin
3rd Year Class

Grace Alexander, MD
Rush Medical College
Tristan Bakerink, MD
University of Nevada Las Vegas

Adam Blaine, MD
University of Washington

James Burton, MD
University of Louisville

Paige Carlson, MD
University of Minnesota

Hunter Frederiksen, MD
University of Utah

Lakshmi Guduguntla, MD
Wayne State

Brittnee Haynes, DO
Idaho College of Osteopathic Medicine
(Medicine-Psychiatry)

Darlene Julian, MD
University of Nevada Las Vegas

Monica Knaack, MD
University of Iowa

Tyler Maggio, MD
Southern Illinois University

Taryn Nishimura, MD
University of Iowa
(Medicine-Psychiatry)
Kimiya Nourian, MD
University of Utah
Marcus Osman, MD
University of North Dakota

Joe Phillips, MD
Georgetown University

Zeke Quittner-Strom MD
University of Texas San Antonio
Alyssa Ray, MD
Southern Illinois University

Natalie Ross, MD
University of Iowa

Joe Salomone, MD, PhD
University of Cincinnati
PSTP

Ashten Sherman, MD
University of Iowa
PSTP and StARR Scholar

Laurel Smeins, MD
University of Iowa

Mike Tabet, MD
University of Vermont

Megan Vree, MD
University of Iowa

Mackenzie Walhof, MD
University of Iowa
Patrick Watson, MD
Indiana University

Alice Xu, MD
University of Cincinnati
4th and 5th Year Classes

Sarah Little, MD
West Virginia University – Charleston
(Medicine-Psychiatry)

Shivali Patel, MD
Rush University
(Medicine-Psychiatry)

Antony Gout, MD (R4)
University of Iowa
(Medicine-Psychiatry)

Alicia Kilian, MD (R4)
University of Minnesota
(Medicine-Psychiatry)
Department Contacts
For information regarding Categorical and Preliminary Programs contact:

Cindy K. Batzkiel
Program Administrator
Department of Internal Medicine
200 Hawkins Dr., E326-2 GH
Iowa City, IA 52242
Phone: (319) 356-2034
FAX: (319) 384-8955
Email: intmedres@uiowa.edu

Abbey Gilpin
Associate Program Administrator
Department of Internal Medicine
200 Hawkins Dr., E321 GH
Iowa City, IA 52242
Phone: (319) 384-7093
FAX: (319) 384-8955
Email: intmedres@uiowa.edu

Stacy Sueppel
Program Coordinator
Department of Internal Medicine
200 Hawkins Dr., E323 GH
Iowa City, IA 52242
Phone: (319) 384-9668
FAX: (319) 384-8955
Email: intmedres@uiowa.edu
Residency Program Administration

Manish Suneja, MD
Vice Chair for Education
Director, Residency Program
Department of Internal Medicine

Andrew Bryant, MD
Associate Director, Residency Program
Department of Internal Medicine

Brian K. Gehlbach, MD
Associate Director, Residency Program
Department of Internal Medicine

Krista Johnson, MD
Associate Director, Residency Program
Department of Internal Medicine

Justin Smock, MD
Associate Director, Residency Program
Department of Internal Medicine

Mark C. Wilson, MD, MPH
Associate Dean, Graduate Medical Education
Department of Internal Medicine

Jenny Strouse, MD
Assistant Director, Residency Program
Department of Internal Medicine

Carly Kuehn, MD
Educational Director, Safety and Quality
Department of Internal Medicine

Matt Soltys, MD, MME
Mentor, VA Safety and Quality
Department of Internal Medicine

Jane S. Rowat, BS, MS
Education Development Director
Department of Internal Medicine
Medicine-Psychiatry Program
Andrea Weber, MD, MME
Director, Medicine-Psychiatry Residency Program
Departments of Internal Medicine and Psychiatry

Vicki J. Kijewski, MD
Associate Director, Medicine-Psychiatry Residency Program
Departments of Internal Medicine and Psychiatry
Physician Scientist Training Pathway (PSTP)

David Stoltz, MD, PhD
Director, Physician Scientist Training Program
Department of Internal Medicine
Chair and Department Executive Officer
 This is an extraordinary time in your life, a transition that marks the beginning of a crucial new period in your professional career and in your personal experience. When I went about interviewing for and choosing my residency, I was a bit anxious but mostly very excited. I knew it would be hard work, but I looked forward to the challenge as I am sure you do now.
This is an extraordinary time in your life, a transition that marks the beginning of a crucial new period in your professional career and in your personal experience. When I went about interviewing for and choosing my residency, I was a bit anxious but mostly very excited. I knew it would be hard work, but I looked forward to the challenge as I am sure you do now.
I sincerely believe that you stand at the beginning of one of the most exciting times in the history of medicine. After decades of research in human disease we have begun to see a novel array of new therapies that will rapidly expand in the near future. The Department of Internal Medicine at the University of Iowa has contributed in countless ways to this new world of discovery, remedy, and hope. As interim chair of the department, my goal is to ensure that we remain in the forefront not just of change but of important science, meaningful education, and the best patient care available anywhere -- all of this in a stimulating environment of cultural and intellectual diversity.
Among my highest priorities is to see that our residency program continues in its position as one of the premier programs in the nation. Dr. Manish Suneja and his team spearhead this effort, maintaining a training curriculum and a learning environment that thoroughly prepares you for the next level in your career. At the same time, we are committed to helping you learn how to preserve a meaningful balance between work and home, a skill that will shape every part of your life.
I foresee tremendous growth and unlimited possibilities in internal medicine at Iowa, and I urge you to join us in Iowa City. In this remarkable and heterogeneous community, you'll find the breadth, depth, and diversity of patients and world-renowned and caring faculty and staff, and outstanding facilities to make your education a success. Look over our website, visit Iowa City, and compare us with other programs. Don't hesitate to contact Dr. Suneja or me if you have questions about Iowa City or about internal medicine at the University of Iowa.
Upinder Singh, MD
Chair & Department Executive Officer
Department of Internal Medicine
Professor of Medicine
Internal Medicine Faculty
By Division
Cardiovascular Medicine
Endocrinology and Metabolism
Gastroenterology-Hepatology
General Medicine
Hematology, Oncology, and Blood & Marrow Transplantation
Immunology (formerly the Divisions of Allergy-Immunology and Rheumatology)
Infectious Diseases
Nephrology and Hypertension
Pulmonary, Critical Care, and Occupational Medicine
Program in Bioinformatics and Computational Biology
How to Apply
Apply using the Electronic Residency Application System (ERAS), and register with the National Resident Matching Program (NRMP).
We accept applications September 15 through December 31, and selected candidates will be invited to interview. We recommend you apply early.
A limited number of categorical positions are occasionally available at the PGY-2 level.
We welcome applicants who will graduate from qualified medical school programs in this country or abroad. Please note our eligibility criteria.
Thank you for your interest in our program. If you have any questions, please contact us at intmedres@uiowa.edu or (319) 384-9668.
Training Program Eligibility Criteria
U.S. Allopathic Medical School Graduates
- Completed USMLE Step 1 and 2
- Application via the Electronic Residency Application Service (ERAS) including:
- A minimum of three letters of recommendation
- Dean’s letter (MSPE)
- Medical school transcript
- Personal statement
- Photograph (optional)
Osteopathic Medical School Graduates
- Completed COMLEX Step 1 and Step 2 OR USMLE Step 1 and 2
- Application via the Electronic Residency Application Service (ERAS) including:
- A minimum of three letters of recommendation
- Dean’s letter (MSPE)
- Medical school transcript
- Personal statement
- Photograph (optional)
International Medical School Graduates
- Completed and passed USMLE Step 1, Step 2, and Step 2 CS on first attempt. Scores must be available before you can be considered for an interview.
- Hands on Clinical Experience in the United States medical system (this does NOT include observerships)
- Application via the Electronic Residency Application Service (ERAS) including:
- A minimum of three letters of recommendation
- Dean’s letter (MSPE)
- Medical school transcript verifying appropriate medical education to train in a large teaching hospital
- Personal statement
- Photograph (optional)
- U.S. citizenship or J-1 Visa
The Interview
We will virtually interview selected candidates October through January. The night prior to your interview, we will be holding a Zoom “Happy Hour” with current residents. This is an informal time to get to know our residents and learn more about the program and life in Iowa City. You will receive a personalized itinerary prior to your scheduled interview. Your day will start with an overview of the program, followed by interviews with our program director, an associate program director, and a member of the UIHC faculty. Between interviews, there is also a virtual tour of the University of Iowa Hospitals and Clinics, and a time to chat with our current chief residents. Following your interviews, you will join our residents for our Noon Conference and participate in a Chief Resident led Case Conference. After conference, there will be a short wrap up; we plan for the day to end by 2:30 p.m.