How ethnically diverse are your patients?
Like a lot of university towns, we have a large international community. Growing cultural diversity is another reason Iowa City is an interesting place to live. Diversity is embraced and celebrated with city and university events, festivals, clubs and programs. The University works hard to recruit and retain minorities with its affirmative action policies. About 13% of Iowa citizens are non-white as are almost 13% of the patients seen in our pediatric clinic.
Are there any job opportunities for my spouse/significant other?
Yes, in June 2016, Iowa City had an average of 3.2% unemployment. Also check out The University of Iowa's Dual Career Services.
Is it possible to do an international elective in your program?
Yes! Residents can do International Health Electives in PGY2 and/or PGY3.
What are the fellowship opportunities available?
We currently have 29 fellows training in our 10 accredited fellowship programs.
Is this a family friendly program?
Yes! We love children and support residents in their efforts to balance work with family life. We have several dual physician resident and faculty families and understand the stresses. Women residents receive up to 6 weeks of paid maternity leave after delivery. Men get 5 working days off for paternity leave. The house staff health insurance policy provides full coverage for spouses and children. There are several childcare facilities near the hospital and one on-site. The training program also has activities during the year where all family members are invited, such as our annual resident picnic.
[Lab research] Is there sufficient patient volume so that I can have multiple exposures to a variety of diseases?
With 5,400 annual inpatient pediatric admissions and over 218,000 outpatient encounters you will see plenty of the most common illnesses and trauma that children experience and plenty of the "zebras" as well. Our clinical practice serves the general pediatric health care needs of the local community and the subspecialty needs of the region. Our department receives referrals for specialized services from neighboring states as well.
Patients are referred from across the nation for certain specialized pediatric treatments and services, such as bone marrow transplantation, pediatric cardiology, otolaryngology, neurosurgery and orthopedics. In addition, we conduct clinics in other cities and towns throughout Iowa. Our patients represent all pediatric age groups and all socioeconomic strata and they present with virtually all acute and chronic conditions.
What is the program's balance between primary and specialty care?
We seek to provide each resident physician with a sufficiently broad experience that he or she can choose wisely among all the pediatric options to pursue a career in the general practice of pediatrics, a subspecialty service career or an academic career. About half of our graduates go on to practice general pediatrics while the other half go on to fellowships in pediatric subspecialties or academic pediatrics.
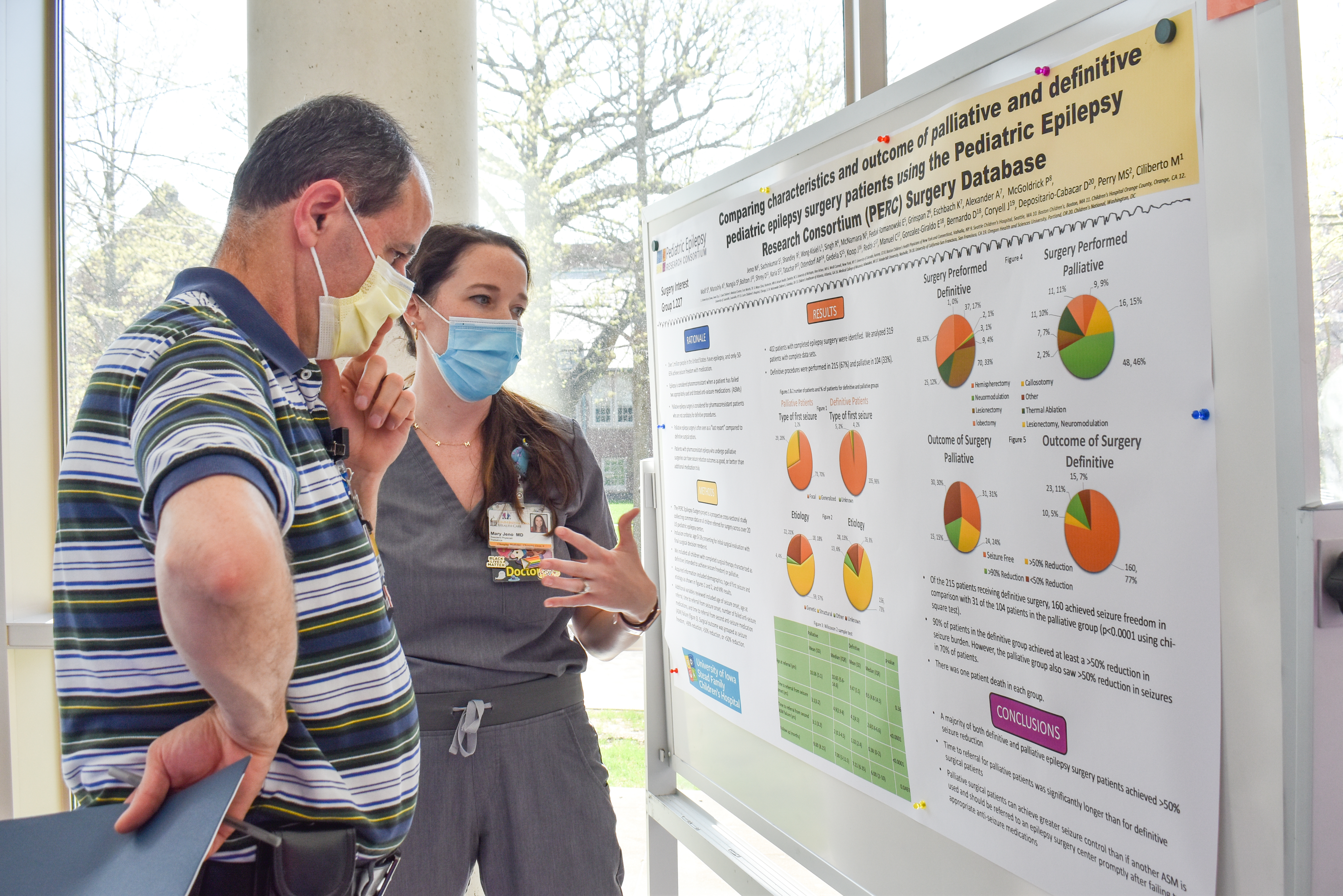
Do you have a research project requirement for graduation?
While we do not have a requirement to complete a research project, we do encourage residents to work on bench or clinical research projects along with our faculty. The Stead Family Department of Pediatrics ranks 13th in public institutions for NIH funding and we have 2 Howard Hughes research investigators in our department. Two of our residents have won the prestigious Society of Pediatric Research's Resident Research Awards in the past couple of years.
If you have additional questions please contact our program coordinator at peds-res@uiowa.edu.

















 By the Numbers
By the Numbers









 f Iowa Stead Family Children's Hospital
f Iowa Stead Family Children's Hospital
 North Liberty Clinic
North Liberty Clinic

























































 If you are interested in applying to the Pediatric Residency Program, applications are accepted only through
If you are interested in applying to the Pediatric Residency Program, applications are accepted only through 