Iowa has historically been a pioneer in offering training programs that reflect the health care needs of the nation and the world.
Launching career successes for our residents and fellows is done by design. We actively work to provide rigorous yet flexible programs in an environment of support and collaboration.
Graduate Medical Education - By The Numbers
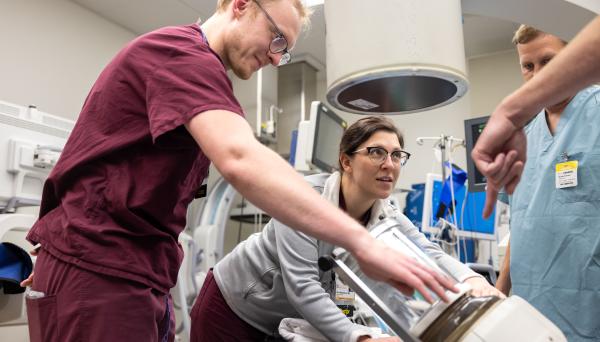
Iowa provides the balance you’re looking for in a residency program. We’ll expose you to the complex cases, state-of-the-art technology, innovative research, and hard work that define your success as a physician.
You’ll be working with some of the most gifted clinicians and researchers in your chosen field as well as expert colleagues from related disciplines. Our well-established fellowships will expose you to cases and techniques that prepare you for your career as a medical specialist.
Learn More
Iowa Practice Opportunities
The Office of Statewide Clinical Education Programs (OSCEP) connects physicians and Iowa practices through the Iowa Practice Opportunities Directories.