The Internal Medicine and Psychiatry Combined Residency Program at the University of Iowa is a 5-year program that offers residents the opportunity to provide comprehensive care to patients with comorbid medical and psychiatric conditions.
Clinical Opportunities
The development of our residents into well rounded physicians is the core of the University of Iowa Internal Medicine residency mission. This growth happens by taking care of patients in clinic and at beside.
Our program utilizes an X+Y schedule that allows for abundant patient care-experiences in both the inpatient and outpatient settings with increasing levels of autonomy as residents progress through their training. Our residents rotate for 4 weeks on an inpatient general medicine service or subspecialty consult service followed by a 1 week experience dedicated to ambulatory medicine (the Y week). This system allows for significant individualization of schedules so residents can pursue their interests in specific subspecialties or explore many different subspecialties as they decide if they want to go into a specific subspecialty or become a general internist.
If you are interested in doing a preliminary year at the University of Iowa or our medicine-psychiatry residency program, please check out the links below.
We invite you to take a tour of where you will be learning medicine by checking out our facilities.
X-Block
During the 4-week X-block, our residents rotate through core rotations that expose residents to the full breath of inpatient general medicine and a wide variety of elective rotations that provide ample flexibility for residents to tailor their experience to their career goals.
Core Inpatient Rotations
The foundation of the experience that develops our residents from medical students into independent physicians is the experience of taking care of patients on our general medicine wards. Our residents rotate on general medicine teams at the University of Iowa Hospitals and Clinics and the Iowa City VA. We offer a primary cardiology inpatient team at the University and our residents also have the opportunity to rotate on the medicine/psychiatry unit as senior residents. Our residents also get plenty of ICU experience while rotating in the Medical Intensive Care Unit and Cardiovascular Intensive Care Unit.
During the first year, our residents generally spend 6 to 7 X-blocks on a core rotation.
Our residency prioritizes the experience of one team taking care of patients from admission until discharge. Therefore, none of our core rotations have an “admitting team” and a “floor team.” Every team both admits patients and takes care of them on the floor until they discharge. We believe facilitates residents getting to know their patients personally and develop relationships with them and that is crucial to our residents growth as clinicians.
UIHC Inpatient Medicine
The University of Iowa Hospitals and Clinics (UIHC) is the only academic hospital in the state of Iowa. Consequently, many of our patients present from across the state with complicated and/or rare medical problems requiring the subspecialty care that only our institution can provide. UIHC also acts as the “safety net” hospital for the state of Iowa, providing care to the under-served populations. As such, our residents see a wide range of conditions in a diverse patient population while rotating on the general medicine floor at UIHC.
Three teams, each comprised of a staff hospitalist, one senior resident, three interns, and 2-3 medical students admit, diagnose, and manage these patients. Two interns take care of patients during the daytime and the third intern provides coverage at night every time their team is on call. On average, interns take 3-4 nights of call per X-block.
Admission are allocated based on a rotating call cycle of a “pre-call,” “on-call,” and “post-call” team. No patients are admitted to the “post-call” team.
Recently (as of April 2023), UIHC geo-localized all of the inpatient services. This means all general medicine teaching team patients are now almost entirely located on the same floor – just a couple steps from the team room. This also provides for great continuity of care as our residents now work with the same set of nurses, social workers, pharmacist, physical therapists, and occupational therapists, which allows our residents to work together more closely with the support staff and learn from them as they provide outstanding patient care.
There is also an ultrasound machine on the general medicine floor that is easily accessible and readily available for point-of-care ultrasound exams and performing bedside procedures.

Iowa City VA Inpatient Medicine
The Iowa City VA Medical Center is a 3 minute walk away from UIHC and it provides a fantastic learning opportunity for residents. Patients come from a wide range of socioeconomic status’ and backgrounds and they present with a wide variety of medical problems, that range from “bread and butter medicine” to the “zebras”.
The ICU at the VA is also an open ICU that is staffed with a pulmonary/critical care staff and fellow, which allow our residents to get experience taking care of all levels of acuity.
Three teams, each comprised of a staff hospitalist, one senior residents, two interns, a pharmacist, and 2-3 medical students admit, diagnose, and manage the patients admitted for primary medicine problems to the VA. Admissions are allocated based on a rotating call cycle of a pre-call,” “on-call,” and “post-call” team. No patients are admitted to the “post-call” team. The interns work schedule is a rotating schedule with interns covering three days in a row on the pre-call, on-call, post-call cycle. Then the intern transitions to nights and covers the night call shift into the post-call day before starting the call rotation back on days. Overall, interns do an overnight call every 6th night.
Cardiology Inpatient Teaching Service
Comprised of a staff Cardiologist, a senior resident, and two interns, the inpatient cardiology team diagnoses and manages patients with acute cardiovascular illness who do not require an ICU admission. Common problems seen on this service include acute coronary syndromes, decompensated heart failure, valvular disease, pulmonary hypertension, pericarditis, and endocarditis. The team admits patients daily. Overnight, cross-coverage and new admissions are managed by our night float team.

Medicine/psychiatry unit
The medicine/psychiatry unit at UIHC is a 15 bed unit. Residents on this rotation get experience managing the complex interactions between psychiatric and medical illnesses. One team, comprise of a Medicine staff and Psychiatry staff, one senior resident, and two interns care for up to a total of 15 patients who have both a medical indication for hospitalization and a psychiatric indication for hospitalization. The team admits patients daily with no overnight call. Overnight admissions and cross cover are provided by the night float team.
If you are interested in a combined Internal Medicine and Psychiatry Residency, please visit their residency page: https://gme.medicine.uiowa.edu/internal-medicine-psychiatry-residency
Medical Intensive Care Unit (MICU)
The UIHC Medical Intensive Care Unit (MICU) is a 26 bed unit. Common problems managed in the MICU include sepsis/shock, acute and chronic respiratory failure, and other critical conditions.
Two teams, each comprised of a Pulmonary/Critical Care staff, fellow, and 2 senior residents, 1 intern, and 1 APP help provide care to the patients admitted to the MICU. The intern on the team gains experience taking care of critically ill patients by helping to admit patients and provide cross-coverage every other night. Interns do not have any day coverage responsibilities in the MICU. The senior residents take call every fourth night with one day off per week.
Throughout this rotation, residents will have plenty of opportunity to perform beside procedures including central line placement, paracentesis, thoracentesis, lumbar puncture, and arterial line placement. Point-of-care ultrasound is a highly emphasized aspect of this rotation and residents have ample opportunity to get hands on experience obtaining images and measurements at bedside.

Cardiovascular Intensive Care Unit (CVICU)
The UIHC Cardiovascular Intensive Care Unit (CVICU) is a 24-bed unit. Common problems seen on this service include cardiogenic shock, STEMIs, severe valvular dysfunction, and life-threatening arrhythmias.
Patients admitted to the CVICU are either admitted to the medical team, if their primary problem is a medical cardiovascular problem, or to the surgery team. Four senior internal medicine residents help staff the medical team of the CVICU, along with a staff cardiologist and cardiology fellow. Each resident takes call every fourth night with one day off per week.
During their rotation on the CVICU, residents will become comfortable with the interpretation of hemodynamic monitoring number from PA catheters (Swan-Ganz catheters) and the management of cardiac assist devices including intra-aortic balloon pumps (IABPs) and impellas.

Night Float
The night float team consists of two pairs of one intern and senior resident. Each pair works every other night. This team helps to cross-cover and admit to the Inpatient Cardiology Teaching Service and the Medicine/Psychiatry Unit. The senior resident also covers Surgical co-management (general medicine) consults.
Elective Rotations
The elective rotations allow for residents to spend a dedicated 2- to 4-week block time immersing themselves in a specific sub-specialty to explore their future career interests and deepend their knowledge in the core subspecialities of medicine.
We also have many medicine-adjacent rotations that residents rotate on to explore their other interests.
Subspecialty consult and clinic services:
- Allergy/Immunology
- Acute care clinic
- Cardiology
- Endocrinology
- Gastroenterology
- Geriatrics
- Hepatology
- Hematology
- Infectious Disease
- Oncology
- Palliative care
- Pulmonology
- Nephrology
- Rheumatology
- Surgical-co management (general medicine consults)
Unique clinical opportunities:
- International Health (link to international health page)
- Addiction medicine
- Anesthesia
- Bone marrow transplant (primary service)
- Dermatology
- Hospitalist rotation
- Malignant hematology (primary service)
- Neurology stroke service (primary service)
- Sports medicine
- Transplant hepatology
- Transplant nephrology (primary service)
- Visiting resident at a hospital outside the VA and UIHC
Unique opportunities beyond patient care:
- Research elective
- Teaching resident rotation
- Course on EKG interpretation
- Health informatics
Hospitalist Rotation
The hospitalist rotation pairs residents interested in hospitalist medicine with a staff working on a “hospitalist only” service. We have a partnership with St. Luke’s hospital in Cedar Rapids, so residents have the opportunity to experience the day-to-day workflow of a hospitalist firsthand in either a community or academic setting, if the resident wished to stay a UIHC.
Y-Week
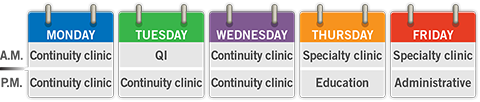
During the Y-week, our residents learn the key skills of taking care of patients in the outpatient setting. Residents participate 5 half days of Continuity of Care Clinic, 2 half days in a subspecialty clinic, 1 half day dedicated to working on their quality improvement curriculum, 1 half day of administrative time, and 1 academic half day dedicated to resident education.
Continuity of Care (COC) Clinic
Residents spend five half days in their Continuity of Care (COC) Clinic at the VA or IRL. This clinic presents an opportunity to build personal panel of patients over 3 years of residency. Residents are responsible for acute clinic problems, chronic disease management, and preventative care.
Residents can also elect to spend a half day in the Iowa City Free medical clinic or the LGBTQ clinic as one of their 5 COC clinic days.
Specialty clinic
Residents rotate in 2 different subspecialties. Subspecialities that match the residents career goals and interests are prioritized. Residents often work with the same staff during their Y-week specialty clinic, which allows for the development of a mentor-mentee relationship between staff and residents. Residents interested in research often end up doing research with their Y-week subspecialty staff or end up being connect to a research project by their Y-week subspecialty staff.
Quality Improvement half day
Every resident participates in a group QI project. The group that you work with is your Y-week cohort. During each Y-week, there is a half day scheduled for the resident to work on tasks related to their QI project.
Administrative half day
This is time set aside in your schedule to catch up on the administrative tasks of being in clinic. Residents use this time to finish up notes and call patients with results. Many residents also use this time to catch up on things outside the hospital like haircuts, dental appointments, and going to see their own doctor.
Academic half day
This is when residents participate in Ultrasound Curriculum, Quality Improvement, Resident Teaching Skills Curriculum, Board Review Curriculum, RRT/Code Blue Simulation, and Ambulatory Workshops.
It’s also a great time to spend time with your co-residents.
For more information about the education half day or the curriculum mentioned above, please visit the Residents as Learners section.
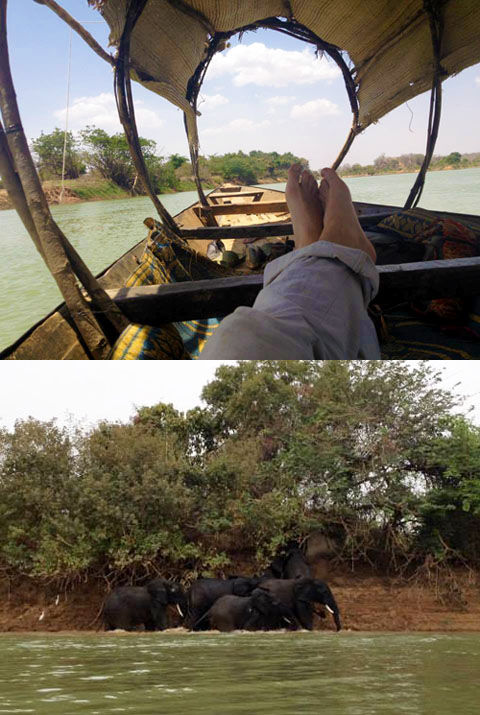
International Health
The Internal Medicine Residency at Iowa offers international health rotations through our international partners. These rotations are intended to give the participating residents a more global perspective in cultural, social, economic, and political issues of another country that impact the nation’s healthcare system. Two of our residents will be participating in an international health rotation in Uganda, mentored by Dr. Robert Blount, in February of 2024. This will be our first international health rotation since COVID!
We also have established connections in India, Ghana, and Niger. You can read about our residents experiences at these sites from pre-COVID times below.
For questions regarding an international health rotation during residency, please contact the Residency Program at intmedres@uiowa.edu.
Dr. Maria Story: "I went to Lady Willington Hospital in Manali, India during my third year of residency for 4 weeks. Manali is a rural hill station (small town) in the state of Himachal Pradesh in north central India."
Dr. Josiah Zubairu: I spent 2 weeks in the village of Agbozume, Volta Region in Ghana in the Spring of 2017 during my 3rd year of residency. This was my second time visiting and providing healthcare to this community of mostly farmers and traders.
Dr. Juan Caraballo: I spent the last 3 weeks and a half in Niamey, Niger. Niger is a landlocked country in West Africa. I worked under the supervision of Dr. Susan Beebout in the Clinique Olivia, a clinic in a poor part of the city associated with Evangelical Church of Niger.
India International Rotation
I went to Lady Willington Hospital in Manali, India during my third year of residency for 4 weeks. Manali is a rural hill station (small town) in the state of Himachal Pradesh in north central India. The Lady Willingdon Hospital is a Christian mission hospital that has been serving the local community since 1935. The catchment area is extremely broad, serving patients up to 10 hour drive on poor quality mountainous dirt roads since there is minimal medical infrastructure in the this area (Himalayan Mountains).
I stayed on the hospital campus (they have small rooms available for rotating trainees) and there were several students from the UK also doing an elective rotation. In the morning we did hospital rounds on infants and children, patients hospitalized for medical conditions, and post-surgical patients. In the late morning and through the afternoon we did outpatient clinic, which was essentially an acute care clinic. There is very little chronic disease management or focus on health prevention. Basic laboratory testing and X Rays were available when absolutely indicated. There is also a labor and delivery room (which I did not participate much in, given that I was an Internal Medicine trainee) and an 24-hour Emergency Department.
I saw a wide variety of illnesses, including TB, Scrub Typhus, Entamoeba histolytica, dysentery, a variety of worm infections, and typical bacterial pathogens. There was a high number of accident-related injuries, primarily from MVA’s and unsafe work conditions. Older people presented with respiratory symptoms, probably from some form of obstructive lung disease from smoke exposure from cooking fires and inhaled dust/dirt from hard labor.
Throughout my elective, I was impressed that the staff at Lady Willingdon Hospital were able to provide excellent care with minimal resources by our standards. I did experience a degree of ‘culture shock,’ but overall it was a very valuable experience and I am thankful for the opportunity to travel to India during residency. I felt safe throughout my time in Manali, the scenery was amazing, and I had the opportunity to meet many wonderful people.



Ghana International Rotation
I spent 2 weeks in the village of Agbozume, Volta Region in Ghana in the Spring of 2017 during my 3rd year of residency. This was my second time visiting and providing healthcare to this community of mostly farmers and traders. It was very positive experience for exposure to clinical work, community education and understanding disparities in healthcare access. I was exposed to multiple array of interesting pathology and medical cases, some with very limited resources for further evaluation and management. I had to make grasp of whatever limited options I had to pursue care of these people. Exchanging ideas with local physicians and people in the community was also very educative. I plan to continue to visit Agbozume.
I am thankful that the medicine department could support me in many ways for my trip to Ghana. I will encourage many others with interest in International Health to consider this tremendous opportunity.

Niger International Rotation
I spent the last 3 weeks and a half in Niamey, Niger. Niger is a landlocked country in West Africa. I worked under the supervision of Dr. Susan Beebout in the Clinique Olivia, a clinic in a poor part of the city associated with Evangelical Church of Niger. During my time in Niger I had the unique opportunity to work with an underserved population and with limited resources. I had the opportunity to see and help a broad spectrum of patients with a broad spectrum of pathologies, including diabetes and hypertension, typhoid, tuberculosis, sickle cell disease and many more. I would see around 10-12 patients daily with the help of a medical assistance that will also serve as translator. Most patient speak only their native language (Hausa, Zarma) and only around 20% speak French. Only very limited labs were available and most patients were not able to afford extensive diagnostic work up.

Practicing in an environment where laboratories test and imaging are not readily available I learned to trust my history taking and physical exam, and to formulate a clinical assessment with just limited information. Having to serve a population with limited resources strengthen my resourcefulness and taught me about cost-effectiveness in a very direct and practical way.

During my rotation in Niger I had the opportunity to spent one week at the National Hospital of Niamey, where I was part of the team taking care of 32 patients in the women general ward. I learn about the logistics of patient care and education in a teaching hospital and the day to day life of my colleagues residents in Niger. Even though the National Hospital is one of the main three hospitals in Niamey, the capital of Niger, there are no ventilators, angiography or MRI, and most medications routinely used in US are not available there, at all. Being able to see the highest level of care that is available in one of the poorest countries in the world, compared with United States, was a humbling and enlightening experience that I feel fortunate to have had and I m positive it has enriched me no only professionally but personally.
LGBTQ Clinic
Our residents can elect to provide care in the LGBTQ clinic in the place of one of the half days of Continuity of Care clinic. The LGBTQ clinic provides welcoming and affirming care for all patients. Residents in this clinic learn about the unique aspects of providing healthcare to the LGBTQ population while also learning about the challenges faced by the LGBTQ population from across the state of Iowa and how this affects their access to healthcare.
Please check out the LGBTQ clinic website for more information.
Iowa City Free Medical Clinic
Our residents can elect to provide care in the free medical clinic as one of their five half days of Continuity of Care clinic. Residents who rotate at the free medical clinic get first hand experience in helping the underserved communities in the Iowa City area and learning about the challenges they face in accessing healthcare.
Please check out the Free Medical Clinic website and the Distinction in Health Equities.
MAT Clinic
Residents can care for people with substance use disorders (SUD) by electing the Medications for Addiction Treatment (MAT) clinic as one of their elective or continuity clinic experiences. Residents who spend time in the MAT clinic get clinical exposure in starting and managing evidence-based medications for SUD. They will support patients through early and established recovery, screen and treat for concurrent medical and psychiatric comorbidity, and advocate for patients as they intersect with other non-healthcare institutions encountered by people with SUD.
Preliminary Year
A one-year program is available for candidates who require Internal Medicine training prior to starting another specialty. We treat our preliminary residents the same as we do our categorical residents. Our prelims participate in the same orientation as our categorical residents, they are invited to all of our didactic conferences, and all of our residency’s social events outside of the hospital. The year culminates with a graduation ceremony that celebrates the 3rd year categorical residents’ graduation and also our prelims graduation as they move on from the IM program to their respective specialty of choice.
We also work with our prelims to individualize their schedule as much as possible to maximize the applicability of their rotations to their future career specialty. The major difference between the prelim schedule and the categorical schedule is there is no Y-week, only 4 week blocks of rotations.
For more information on our prelim year, please reach out to intmedres@uiowa.edu.