About the Program
We are convinced our people, our approach, our facilities, the ease of living in Iowa City, and our quality of training can all make a difference in your career.
We invite you to consider the advantages of choosing Iowa for your Emergency Medicine training.
Quick facts
- 10 residents are accepted each year.
- 30 total residents are ACGME approved for our training program.
- The University of Iowa Health Care Emergency Department (main training site) sees greater than 50,000 patients per year with a 35% percent admission rate with 5% admitted to an Intensive Care setting.
- St. Luke’s Medical Center Emergency Department (community training site) sees greater than 50,000 patients per year with a 20% admission rate with 2% admitted to an Intensive Care setting.
Rotations
- All required Emergency Medicine and other required rotations are scheduled at the UI Health Care on University Campus or at St. Luke’s Medical Center in Cedar Rapids, Iowa. St. Luke’s is an approximate 30 minute drive from the University of Iowa (25 miles).
- Elective rotations can be scheduled at the UI Health Care, or in a number of other locations including internationally.
- Our third year emergency medicine residents have the opportunity to serve as flight physicians in Iowa's 40-year-old Air and Mobile Critical Care Services Program. They response to the scene of motor vehicle accidents and other major traumas. They also participate in the interfacility transfer of patients with conditions such as intracranial hemorrhage, stroke, myocardial infarction, and sepsis. Flight physicians have the ability to perform procedures on flights as well as assist the flight crew with management of these critically ill patients.
- Thanks to the dedicated work of Iowa Emergency Medicine faculty who have been working in Haiti for over a decade, our residents have the opportunity to participate in medical mission trips working with a well-established organization that has strong ties to the rural communities it serves.
Benefits
- Competitive stipends
- Comprehensive medical, dental, hospitalization and pharmacy benefits for residents/fellows and their dependents
- 21 days of annual paid time off
Program accreditation
The Emergency Medicine residency at UI Healthcare University Campus is accredited by the Accreditation Council for Graduate Medical Education. Information specific to program requirements for an emergency medicine training program may be found at the ACGME’s Emergency Medicine Residency Review Committee (RRC).
Program Differentiators
Advantages of our program
- The University of Iowa Emergency Department is number one among academic centers for the shortest waiting times for patients and has strong customer service scores. We will teach you to provide rapid, efficient care to patients while maintaining kind and compassionate service.
- Abundant clinical experience comes from our burgeoning patient census, and more than a fifth of our patients are pediatric.
- University of Iowa is one of the top research institutions in the nation providing unparalleled resources. Our department has many ongoing clinical, basic science, and translational research projects.
- Outstanding, nationally-recognized clinical faculty who have trained all over the country. Teachers who have recognized that University of Iowa is a very special place and have come here to help create a world-class teaching institution.
- We have two dual-boarded emergency medicine and critical care faculty who divide their time evenly between the emergency department and the MICU and SNICU respectively. This allows us to offer our residents unparalleled critical care education, both in the department and during their ICU rotations.
- We have a diverse faculty with diverse interests including critical care, ultrasound, simulation, sports medicine, international medicine, emergency medicine services, and others.
- Our Emergency Department supports a full time clinical pharmacist who assists with patient care and is highly involved in our research programs.
- We have 24-hours a day of full social work support dedicated to the Emergency Department.
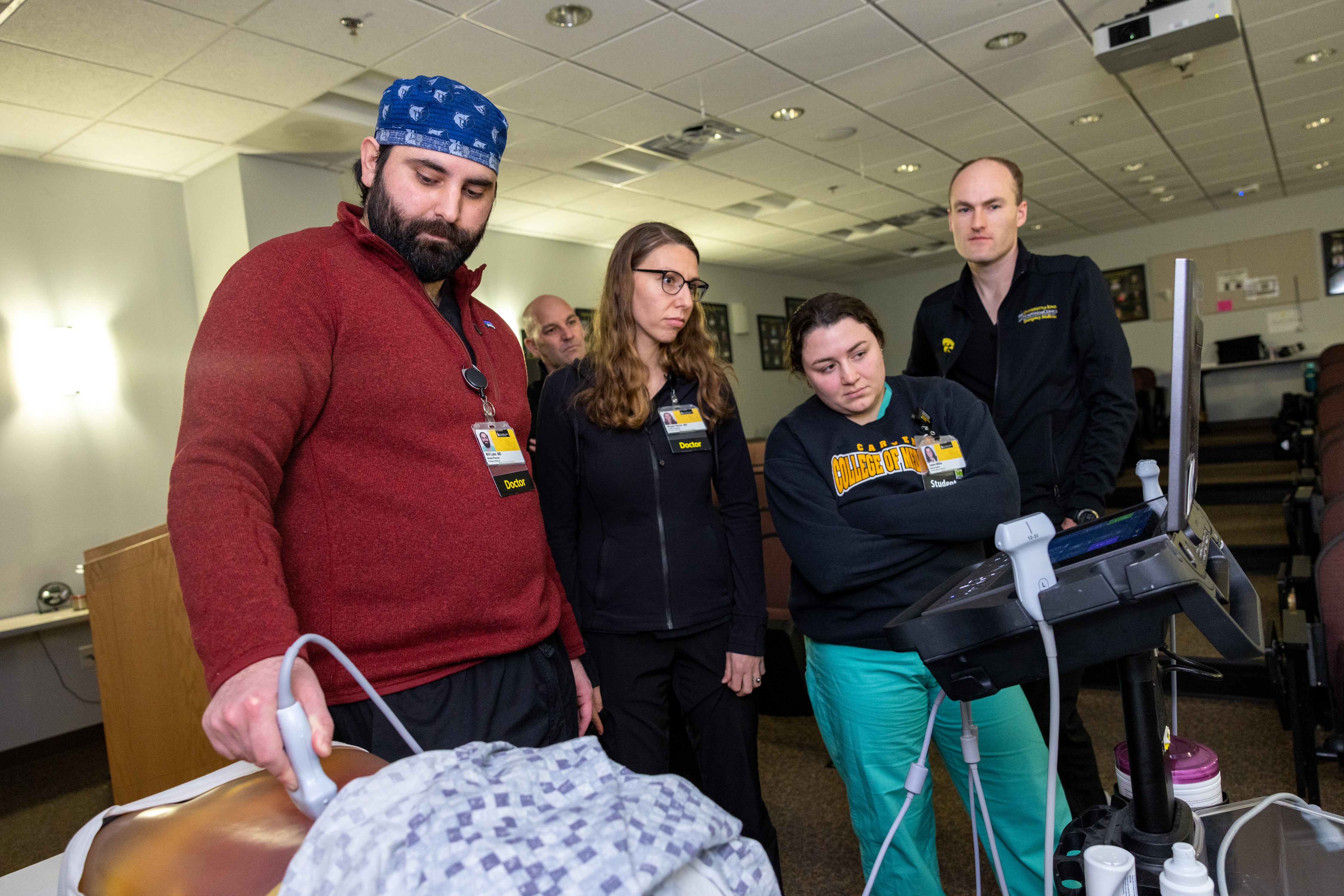
- The use of ultrasound in the practice of Emergency Medicine is expanding exponentially. The University of Iowa Emergency Department recently purchased new, state of the art ultrasound equipment to assist our residents in learning this fundamental skill. The residency program also supports a full time director of the ultrasound curriculum.
Facilities
- State-of-the-art, 60,000 square foot Emergency Department that contains 45 beds.
- Only Level 1 trauma center and burn center in Iowa.
- University of Iowa Hospitals & Clinics is a 711-bed hospital.
Clinical experiences
- The Emergency Medicine residents get a longitudinal EMS experience starting with RAGBRAI medical coverage as interns, followed by event medicine coverage at Iowa Hawkeyes football games, basketball games, and wrestling matches culminating in a month-long EMS month during the third year.
- Our residents learn cutting-edge critical care through dedicated rotations in the Surgical and Neurosciences ICU, the Medical ICU, the Pediatric ICU, the Neonatal ICU, and the Burn Unit at a tertiary academic medical center.
- The opportunity to participate in an ACSME accredited Sports Medicine EMS fellowship at a Big 10 university.
- Fellowships in EMS, Critical Care, Sports Medicine, Academics, Globa Health, Injury Prevention, Research, and Palliative Care.
- Optional Wilderness Medicine course taught mainly in the mountains of Colorado by Iowa faculty.
- Moonlighting available in surrounding community to eligible PGY-3 residents.
- Medical simulation is used extensively within the residency training program. The residency has a full time simulation director who coordinates this area of the residency curriculum. Residents receive training using high-fidelity simulators to augment their clinical experience.
- The residency program has a close relationship with our partner community hospital in Cedar Rapids, with residents spending several months learning there. This allows residents to experience patient care not only in a large academic center, but also at a large community hospital.
Resident Representatives
- EMRA Representative: Nancy Mikati, MD
- AAEM Representative: Kasia Marciniec, DO
- ACEP Representative: Omar Shaban, MD
- House Staff Council: Gigi Landal, MD
- Program Evaluation Committee Members: Nick Lind, MD/Nancy Mikati, MD/Omar Shaban, MD
- Interdisciplinary Committee: Nick Lind, MD/Gigi Landal, MD
Iowa City
- Iowa City is a highly intellectual community with premier arts events that are accessible to residents in terms of cost and location.
- We have an outstanding school system for children in grades K-12.
- A great training program and a high quality of life at an affordable price.
Physician Scientist Training Pathway (PSTP)
The University of Iowa Department of Emergency Medicine Physician Scientist Training Pathway (PSTP) integrates postgraduate clinical and research training to develop physician-scientists who will be future leaders in academic emergency medicine. The PSTP is a pathway within the Emergency Medicine Residency Program and combines graduate medical education with the rich collaborative research community at University of Iowa.
Training at a Glance

The emergency medicine (EM) training program at the University of Iowa Health Care is a three-year program and provides each resident physician with a diverse experience.
To view a synopsis of the training program, please ![]() download our block schedule.
download our block schedule.
Some Elective and Selective rotations are residents have done are: EMS, International, Research, Pharmacy, Nursing, Ultrasound, Toxicology, Critical Care, Community Medicine, Pediatric EM, EKG, Sports Medicine, Opthalmology. With a variety of options residents can specialize their training to fit their areas of interest.
| UI Health Care - University Campus | |
|---|---|
| Rotation 1 | Intro to EM |
| Rotation 2 | EM |
| Rotation 3 | EM |
| Rotation 4 | EM |
| Rotation 5 |
EM (2) |
| Rotation 6 | Ultrasound (1) EM (1) Pediatric EM (2) |
| Rotation 7 | Anesthesia |
| Rotation 8 | Sports Medicine (2) EM Orthopedics (2) |
| Rotation 9 | Trauma |
| Rotation 10 | Pediatric Intensive Care Unit (PICU) (2) Cardiovascular and Thoracic Surgery (2) |
| Rotation 11 | Burns (2) EM (2) |
| Rotation 12 | EM |
| Rotation 13 | Toxicology (2) Quality Improvement (2) |
| EM Weeks: 31 |
| UI Health Care - University Campus | St. Luke's | |
|---|---|---|
| Rotation 1 | EM | |
| Rotation 2 | EM | |
| Rotation 3 | EM | |
| Rotation 4 | EM | |
| Rotation 5 | EM | |
| Rotation 6 | EM | |
| Rotation 7 | EM | |
| Rotation 8 | Obstetrics | |
| Rotation 9 | Medical Intensive Care Unit (MICU) | |
| Rotation 10 |
Surgical and Neuroscience Intensive Care Unit (SNICU) |
|
| Rotation 11 | EM (2) Neonatal Intensive Care Unit (NICU) (2) |
|
| Rotation 12 | Elective | |
| Rotation 13 | Selective | |
| EM Weeks: 30 |
| UI Health Care - University Campus | St. Luke's | |
|---|---|---|
| Rotation 1 | EM | |
| Rotation 2 | EM | |
| Rotation 3 | EM | |
| Rotation 4 | EM | |
| Rotation 5 | EM | |
| Rotation 6 | EM | |
| Rotation 7 | EM | |
| Rotation 8 | EM | |
| Rotation 9 | EM | |
| Rotation 10 | EMS (2) EM (2) |
|
| Rotation 11 | SNICU | |
| Rotation 12 | Elective | |
| Rotation 13 | Elective | |
| EM Weeks: 36 |
Unless otherwise noted, each rotation is 4 weeks.
UI Health Care EM in second and third year will be comprised of both adult and pediatric EM shifts.
Total Number of EM Weeks: 97 Weeks of EM
Total Number of Weeks: 156
Percent Time in EM: 62%
Training Locations
University of Iowa Healthu Care - University Campus
- Patient Volume: >50,000
- Pediatrics represent 18% of total volume
- Trauma represents 22% of total volume
- >35% admission rate with >5% being admitted to an intensive care setting
- Recently constructed, state of the art, 45 bed, 60,000 square foot Emergency Department
- Newly constructed pediatric area
- Level 1 Trauma Center
- Comprehensive Stroke Center
- Specialized trauma, ophthalmologic, dental, and psychiatric rooms
- State-of-the-art ultrasound platforms in the ED
- Advanced imaging modalities located within the department
- Full time dedicated ED based emergency pharmacist support
- Twenty-four hours per day dedicated ED social work support
St. Luke’s Medical Center, Cedar Rapids, Iowa
- Patient Volume: >50,000
- Pediatrics represents 19% of total volume
- Trauma patients represent 15% of total volume
- 20% admission rate with 3% being admitted to an intensive care setting
- Level III Trauma Center
Education/Conferences
The residency supports five hours of weekly educational conference. This time is protected from clinical duty and all residents are expected to attend. An 18-month curriculum is in place that covers the “Model of the Clinical Practice of Emergency Medicine.”

In addition to lectures, the residency incorporates case presentations and small group discussions into the usual content. The Residency utilizes the "Foundations of Emergency Medicine" cases for interactive case discussion. Additionally, there are routinely hands on sessions that include simulation cases (including annual SimWars), procedures labs, ultrasound, as well as mock-oral boards.
The residency supports asychronous learning through the utilization of ROSH Review question based learning as well as utilizing AliemU for online learning resources.
Topic: TEAM Thursday/Board Review
Topic Coordinator: Pomeranz/D. Miller/Shekem
Location: EM Auditorium, 0070 RCP (Elevator F to LL, left off elevator, left at first doorway, through double doors, left at first hallway)
Journal Club
Journal Club is held monthly at a faculty member’s home. The articles are selected by faculty members as well as residents. The objective of journal club is two-fold: to keep up to date on medical literature pertinent to the practice of emergency medicine and to learn the essentials of evidence-based medicine. Food is provided by the faculty host!
Frequently Asked Questions
What are the fellowship opportunities available?
Currently, Sports Medicine, Critical Care Medicine, Emergency Medical Services, and Palliative Care are available. Associate Scholar Fellowships are available in Education, International Medicine, Social Emergency Medicine, Injury Prevention, and Research.
Where is Iowa City?
Iowa City is 220 miles directly west of Chicago on Interstate 80. It’s also within a 4-5 hour drive to Milwaukee, Madison, Minneapolis, Omaha, Kansas City and St. Louis. It has the cultural, educational, social, and political opportunities of a bigger city with the values and ambiance of a Midwestern town. It’s clean, safe, nothing is farther than a 15 minute car ride, it has a great city bus system (with bike racks!), wonderful parks, sports, schools, and even sailing. Those who have lived here and left frequently return because what they were looking for was in their own back yard. But we’re not the only ones who think Iowa City is great:
What’s the weather like in Iowa City?
It depends on what you like. For about two weeks every winter it’s very cold and windy and for two weeks every summer it’s really hot and humid. The rest of the time it’s pretty nice. We have a lot of sunny days even in the winter – 166 per year. Our average snowfall is 28”, average rainfall is 35”, average temperature in the summer is 72.6 and in the winter, 23.7. We consider our weather character building.
What is there to do in Iowa City when you’re not working?
There are 15 different festivals and art fairs, plus concerts and race events. There are many music venues, sports events and neighborhood street fairs and garden walks. We also have a really big mall and several smaller ones, 41 parks, nine golf courses, six public tennis courts, six public pools, some lakes and a reservoir with trails, camping, and boating. There are bike trails, some famous bookstores, a ton of galleries and excellent museums. There are half a dozen or more performing arts venues including Hancher Auditorium. There's always something going on. Find more information from the Iowa City/Coralville Convention and Visitors Bureau.
What’s Iowa City like for kids and families?
There’s ice skating, bowling, organized sports, 50 public parks, miniature golf, a great public library, a toy library, fun centers, swimming pools and three beaches, nine museums including a children's museum, dance companies and public recreation centers that feature many activities for kids and families at little or no cost. We also have 20 movie screens and 50-licensed daycare providers. The Iowa City schools are perennially ranked among the top schools in the nation. Iowa City is unique in the facilities and services available for individuals with disabilities. Many families who have a family member with a disability are reluctant to leave Iowa City because they cannot duplicate those services in another location.
Are there any job opportunities for my spouse/significant other?
Iowa City has a high rate of employment. Check out The University of Iowa's Dual Career Network.
Is it possible to do an international elective in your program?
Yes! Our residents have traveled to Haiti, Indonesia, Vietnam, India, and Tanzania to name a few.
Is this a family friendly program?
Yes! We love children and support residents in their efforts to balance work with family life. We have several dual physician resident and faculty families and understand the stresses. Women residents receive up to 6 weeks of paid maternity leave after delivery. Men get 5 working days off for paternity leave. The house staff health insurance policy provides full coverage for spouses and children. There are several childcare facilities near the hospital and one on-site. The training program also has activities during the year where all family members are invited.
Is there sufficient patient volume so that I can have multiple exposures to a variety of diseases?
Currently, the UI Health Care - University Campus EM Department sees > 60,000 patients per year. Of these, approximately 82% are adults, and 18% pediatrics. Trauma patients represented approximately 22% of our patients, surgical non-trauma 8%, medical 58%, obstetric 5%, and psychiatric 8%. Of the patients seen in the ED, 30% are admitted to the hospital with approximately 4% being admitted to an intensive care unit.
Do you have a research project requirement for graduation?
Yes. Our program requires residents to complete a scholarly activity prior to graduation. We support this through a generous travel allowance to national meetings, a research curriculum, and an experienced research staff. The scholarly activity requirements include:
- A thorough review of the scientific literature relevant to their topic
- Generating a hypothesis research question
- Data collection and analysis
- Development of a publication-quality abstract or manuscript
- Presentation of findings at national, state, regional, or local meeting
If you have additional questions please contact our program coordinator at nicole-hansen@uiowa.edu
Learning Resources
 Simulation and Procedure Labs
Simulation and Procedure Labs
Simulation is a rapidly evolving area of medical education and plays an integral role in healthcare training. Use of simulation for training is uniquely suited to Emergency Medicine given the broad spectrum of illness and pathology encountered and the requirement for proficiency in numerous procedural skills. Management of critically ill patients, efficient use of treatment algorithms, and team leadership skills are only a few of the essential proficiencies that are taught and practiced using medical simulation.
Iowa has dedicated faculty with special expertise and focus on simulation education. The program uses a full family of Gaumard mannequins comprised of infant, child, and adult high fidelity mannequins to meet our diverse educational needs. Case content offers learners the opportunity to encounter a broad variety of clinical scenarios including "bread and butter" emergency medicine cases as well as some specialty scenarios such as mass casualty incidents and skills training with social medicine topics. Faculty and residents will also particpate in and develop skills in strutured debriefing after all simulation scenarios.
During the introduction month for PGY-I, a large amount of time is dedicated to medical, trauma, critical care, and procedural simulation to prepare residents to begin caring for patients in the Emergency Department. Throughout residency, simulation is used to reinforce concepts in patient care and teamwork.
Simulation faculty are continually working to expand the role of simulation for education. In addition to use of simulation during resident conference, the department also participates in in-situ scenarios that take place during clinical shifts and allows the emergency department team to practice together. Residents will also participate in a friendly annual SimWars competition.
Residents with a special interest in simulation are encouraged to work with our simulation faculty to develop simulation-based modules and to conduct simulation or related research that would prepare them to pursue a career in simulation-based education after residency.
Procedure labs are incorporated throughout the residency to augment the procedural skills that residents attain during clinical practice. The residency uses several high and low fidelity “task-trainers” including “The Central Line Man System,” “The Trauma Man System,” and various airway trainers to practice common procedures such as central line placement, chest tube placement, defibrillation/cardioversion and cardiac pacing, paracentesis, thoracentesis, lumbar puncture and basic and advanced emergency airway management. The residents also participate in slit-lamp labs, ENT procedure labs, splinting workshops, and vascular access workshops on a regular basis. The department arranges a cadaver lab annually to practice less common procedures such as thoracotomy, lateral canthotomy, tranvenous pacemaker placement, cricothyrotomy, arthrocentesis, and airway device exchanges.
Organizational Web Sites
Web Sites
The American Academy of Emergency Medicine (AAEM) is the speciality society of board certified emergency medicine physicians, a democratic organization with over 6,500 members. AAEM believes every individual should have unencumbered access to quality emergency care provided by a specialist in emergency medicine. The Academy supports fair and equitable practice environments necessary to allow the specialist in emergency medicine to deliver the highest quality of patient care. Such an environment includes provisions for due process and the absence of restrictive covenants.
The American Board of Emergency Medicine (ABEM) is one of 24 medical specialty certification boards recognized by the American Board of Medical Specialties. ABEM certifies emergency physicians who meet its educational, professional standing, and examination standards. ABEM certification is sought and earned by emergency physicians on a voluntary basis; ABEM is not a membership association.
Founded in 1968, the American College of Emergency Physicians (ACEP) represents more than 28,000 emergency physicians, residents and medical students. Promoting the highest quality emergency care, ACEP is the leading advocate for emergency physicians and their patients, as well as provide CME resources, news, and leadership opportuniites.
Emergency Medicine Residents' Association (EMRA) promotes excellence in patient care through the education and development of emerency medicine residency trained physicians. EMRA is the largest and oldest independent resident organization in the world. EMRA was founded in 1974 and today has a membership of more than 10,000 residents, medical students and alumni.
The Society for Academic Emergency Medicine (SAEM) is dedicated to the improvement of care of the acutely ill and injured patient by improving research and education. To achieve this mission, SAEM influences health policy through forums, publications, inter-organizational collaboration, policy development, and consultation services for physicians, teachers, researchers, and students. SAEM represents excellence and leadership in academic emergency medicine and its values include idealism and quality in all endeavors, nurturing and camaraderie and diversity among members, as well as creative and symbiotic interactions with other organizations.
Fellowships
Learn more about our related fellowships.
- Addiction Medicine Fellowship
- Emergency Medicine PA
- EM Critical Care
- EMS Fellowship
- EM Ultrasound
- Palliative Care/Hospice
- Toxicology
- Sports Medicine
- Social Medicine
- Medical Education
- Research
View all fellowships available at the University of Iowa.

