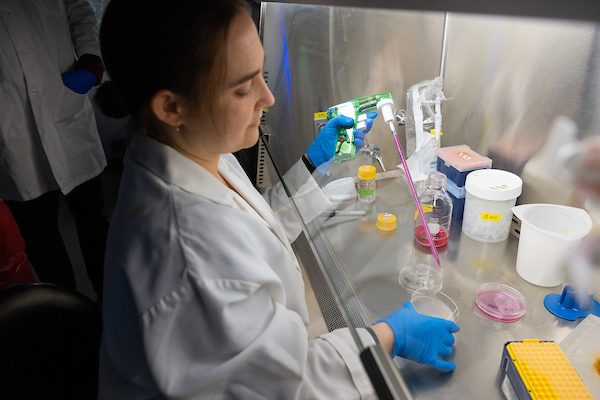
During the first few months of fellowship, we’ll encourage you to meet with several clinical and basic science investigators who have ongoing projects that interest you. We can also help pair you with a mentor whose research interests are similar to yours. Our research mentors are experts in disciplines related to hematology-oncology in the Carver College of Medicine.
Here are some recent mentor and fellow projects:
Mentor: Aaron Boes, MD, PhD
Fellow: Gino Bardi Lola, 2019-2022
Skye J, Bruss J, Toescu S, Aquilina K, Grafft A,
Bardi Lola G, Boes AD. Neuroanatomy of cerebellar mutism syndrome: the role of lesion location. Brain Commun. 2024 Jun 5;6(4):fcae197. doi: 10.1093/braincomms/fcae197. PMID: 39015767; PMCID: PMC11250198.
Mentor: David Gordon, MD, PhD
Fellow: Torin Waters, 2018-2021
Publications:
|
Waters TW, Moore SA, Sato Y, Dlouhy BJ, Sato M. Refractory infantile high-grade glioma containing TRK-fusion responds to larotrectinib. Pediatr Blood Cancer. 2021 May;68(5):e28868. doi: 10.1002/pbc.28868. Epub 2021 Jan 5. PMID: 33403813.
|
|
Waters TW, Dickens DS. Reducing sedated lumbar punctures in pediatric patients with acute lymphoblastic leukemia. Pediatr Blood Cancer. 2021 Nov;68(11):e29272. doi: 10.1002/pbc.29272. Epub 2021 Jul 31. PMID: 34331510.
|
|
Goss KL, Koppenhafer SL, Waters T, Terry WW, Wen KK, Wu M, Ostergaard J, Gordon PM, Gordon DJ. The translational repressor 4E-BP1 regulates RRM2 levels and functions as a tumor suppressor in Ewing sarcoma tumors. Oncogene. 2021 Jan;40(3):564-577. doi: 10.1038/s41388-020-01552-0. Epub 2020 Nov 15. PMID: 33191406; PMCID: PMC7856031.
|
|
Waters T, Goss KL, Koppenhafer SL, Terry WW, Gordon DJ. Eltrombopag inhibits the proliferation of Ewing sarcoma cells via iron chelation and impaired DNA replication. BMC Cancer. 2020 Nov 30;20(1):1171. doi: 10.1186/s12885-020-07668-6. PMID: 33256675; PMCID: PMC7706234.
|
Mentor: Miles A. Pufall, PhD
Fellow: Jessica Zimmerman, 2017-2020
Publications:
|
Zimmerman JAO, Fang M, Doumbia B, Neyman A, Cha JH, Thomas M, Hall B, Wu M, Wilson AM, Pufall MA. Deacylcortivazol-like pyrazole regioisomers reveal a more accommodating expanded binding pocket for the glucocorticoid receptor. RSC Med Chem. 2020 Dec 8;12(2):203-212. doi: 10.1039/d0md00278j. PMID: 34046609; PMCID: PMC8127617.
|
|
Hoover A, Zimmerman JAO, Wiese S, Modi A. Evaluation of Empiric Vancomycin for Fevers During High-dose Cytarabine Administration. J Pediatr Hematol Oncol. 2021 Oct 1;43(7):e1010-e1014. doi: 10.1097/MPH.0000000000002073. PMID: 33560084; PMCID: PMC8329102.
|
|
Zimmerman JAO, Sharathkumar A. Severe Anemia and "Splenomegaly". Clin Pediatr (Phila). 2017 Nov;56(13):1266-1269. doi: 10.1177/0009922816684619. Epub 2016 Dec 22. PMID: 28006959.
|
Mentor: M. Nedim Ince, MD
Fellow: Jamie Truscott, 2016-2019
Publications:
|
Li Y, Liu W, Guan X, Truscott J, Creemers JW, Chen HL, Pesu M, El Abiad RG, Karacay B, Urban JF Jr, Elliott DE, Kaplan MH, Blazar BR, Ince MN. STAT6 and Furin Are Successive Triggers for the Production of TGF-β by T Cells. J Immunol. 2018 Nov 1;201(9):2612-2623. doi: 10.4049/jimmunol.1700808. Epub 2018 Sep 28. PMID: 30266770; PMCID: PMC6200631.
|
|
Truscott J, Guan X, Fury H, Atagozli T, Metwali A, Liu W, Li Y, Li RW, Elliott DE, Blazar BR, Ince MN. After Bone Marrow Transplantation, the Cell-Intrinsic Th2 Pathway Promotes Recipient T Lymphocyte Survival and Regulates Graft-versus-Host Disease. Immunohorizons. 2023 Jun 1;7(6):442-455. doi: 10.4049/immunohorizons.2300021. PMID: 37294277; PMCID: PMC10580113.
|
|
Li Y, Guan X, Liu W, Chen HL, Truscott J, Beyatli S, Metwali A, Weiner GJ, Zavazava N, Blumberg RS, Urban JF Jr, Blazar BR, Elliott DE, Ince MN. Helminth-Induced Production of TGF-β and Suppression of Graft-versus-Host Disease Is Dependent on IL-4 Production by Host Cells. J Immunol. 2018 Nov 15;201(10):2910-2922. doi: 10.4049/jimmunol.1700638. Epub 2018 Oct 5. PMID: 30291167; PMCID: PMC6219912.
|
Mentor: Janice Staber, MD
Fellow: Ahmad Al-Huniti, 2016-2019
Publications:
|
Al-Huniti A, Reyes Hernandez M, Ten Eyck P, Staber JM. Mental health disorders in haemophilia: Systematic literature review and meta-analysis. Haemophilia. 2020 May;26(3):431-442. doi: 10.1111/hae.13960. Epub 2020 Apr 19. PMID: 32307801; PMCID: PMC8475067.
|
|
Al-Huniti A, Sharathkumar A, Krantz M, Watkinson K, Bhagavathi S. Discrepant Hemophilia A: An Underdiagnosed Disease Entity. Am J Clin Pathol. 2020 Jun 8;154(1):78-87. doi: 10.1093/ajcp/aqaa024. PMID: 32232366.
|
|
Sande CM, Al-Huniti A, Ten Eyck P, Sharathkumar AA. Impact of the Survey of Inhibitors in Plasma-Product Exposed Toddlers (SIPPET) study and its post hoc analyses on clinical practice in the United States: A survey of Haemophilia and Thrombosis Research Society members. Haemophilia. 2019 Sep;25(5):764-772. doi: 10.1111/hae.13806. Epub 2019 Jul 2. PMID: 31264762; PMCID: PMC7056002.
|
Mentor: Rebecca Benson, MD, PhD
Fellow: Katie Harmoney, 2015-2018
Publications:
|
Harmoney K, Mobley EM, Gilbertson-White S, Brogden NK, Benson RJ. Differences in Advance Care Planning and Circumstances of Death for Pediatric Patients Who Do and Do Not Receive Palliative Care Consults: A Single-Center Retrospective Review of All Pediatric Deaths from 2012 to 2016. J Palliat Med. 2019 Dec;22(12):1506-1514. doi: 10.1089/jpm.2019.0111. Epub 2019 Jun 21. PMID: 31233350; PMCID: PMC6998041.
|
|
Goss KL, Koppenhafer SL, Harmoney KM, Terry WW, Gordon DJ. Inhibition of CHK1 sensitizes Ewing sarcoma cells to the ribonucleotide reductase inhibitor gemcitabine. Oncotarget. 2017 Jun 28;8(50):87016-87032. doi: 10.18632/oncotarget.18776. PMID: 29152060; PMCID: PMC5675612.
|
David Dickens, MD
Fellowship director and clinical professor
David Claassen, MD, PhD
Fellowship assistant director and clinical assistant professor
Alex Bassuk, MD, PhD
Chair, Stead Family Department of Pediatrics