Radiation Oncology Residency
About the Program
A residency in Radiation Oncology in our department exposes you to all contemporary treatment types and delivery modalities. A thorough, progressive approach to residency training embeds you with a faculty member concentrating on the treatment of specific oncologic sites.
Excellent technical training is available through constant exposure to, and a close collaboration with the other specialties related to the treatment of cancer. With close medical physics, dosimetry and nursing support, residents are free to perform their task of patient care.
Residents graduating the program can expect to be employed in private practice or in an academic institution as a faculty member. Our program is pleased to offer both a clinical and a research pathway to prospective residents and benefits from a close relationship with the Free Radical and Radiation Biology Program.
The Iowa City-Coralville Area
America's Best Employer
 Forbes has ranked the University of Iowa Health Care as the No. 7 employer in the health care industry and No. 48 across all industries in the US. This is the fourth year that UI Health Care has featured in the annual listing of top employers.
Forbes has ranked the University of Iowa Health Care as the No. 7 employer in the health care industry and No. 48 across all industries in the US. This is the fourth year that UI Health Care has featured in the annual listing of top employers.
Welcome from the Department Chair
Welcome to the University of Iowa Department of Radiation Oncology!
Our skilled professionals are committed to delivering compassionate patient care, advancing research, and providing education through the integration of radiation medicine, free radical science, physics, and advanced imaging. We cultivate a culture that promotes continuous improvement, staff empowerment, and cutting-edge innovation.
Our faculty and staff deliver exceptional clinical care at the University of Iowa Hospitals & Clinics and across five community-based sites in Iowa, Bettendorf, Burlington, Clinton, Iowa City, and Ottumwa. We are proud of our department's exceptional scores in patient satisfaction. Patients have access to a range of advanced radiation treatment options, including intensity-modulated radiation therapy (IMRT), volumetric modulated arc therapy (VMAT), brachytherapy (high-dose-rate, interstitial, and eye plaque), Gamma Knife stereotactic radiosurgery (SRS) with frame-based and frameless delivery capability, stereotactic body radiation therapy (SBRT), total body irradiation (TBI), total skin electron beam therapy (TSEBT), and intra-operative radiation therapy (IORT) for the breast. We have an active pediatric radiotherapy service with the capability to treat patients under anesthesia. Additionally, our department boasts the only magnetic resonance imaging (MRI)-guided linear accelerator in Iowa, enhancing the precision of radiation treatments.
Our faculty are integral members of body site-specific multidisciplinary oncology groups within the Holden Comprehensive Cancer Center and are nationally recognized experts in their respective disease areas. Our faculty hold leadership positions in prominent organizations such as the American Society for Therapeutic Radiation Oncology (ASTRO), the American Board of Radiology (ABR), Radiation Research Society (RRS), Society of Free Radical Biology and Medicine (SFRBM), and the American Association of Physicists in Medicine (AAPM).
Research is a cornerstone of our department spanning both basic and clinical realms. Laboratory-based investigations delve into a variety of areas including oxidative stress, immune modulation, radiation protection, radiation targeting, and FLASH radiation delivery. We are actively developing patented new technologies including a dynamic collimation system for proton therapy, novel automatic contouring software for tumors and healthy tissues, and novel software and hardware tools for intensity-modulated brachytherapy. Translational research explores the combination of ionizing radiation with high doses of vitamin C, superoxide dismutase mimetics, and carbon monoxide foams. Clinically, we've pioneered gating techniques for patients treated on the MR LINAC.
We actively seek collaboration opportunities with other investigators at the Holden Comprehensive Cancer Center and throughout the University of Iowa scientific and academic community. Fostering partnerships with other University of Iowa departments and colleges is a priority.
Education is a core focus of the department, and we nurture the next generation of students, residents, and fellows. Our trainees gain exposure to the full spectrum of cancer care, from bench to bedside. With engaged mentors and a wide array of clinical experiences and research possibilities, our program offers a robust learning environment for radiation biology, medical, and physics students alike.
For further information about patient care, training, or research programs, please don't hesitate to contact us.
Sincerely,
Chair, Department of Radiation Oncology
Our Program Aims
Aims of the University of Iowa Radiation Oncology Residency Program
We seek to:
- Educate the future generation of physicians and physician scientists in radiation oncology who are dedicated to the advancement of and improvement in the treatment of cancer.
- Prepare residents for independent practice in any clinical or academic setting. Support and accommodate the individualization of training based on the resident’s future career plans.
- Educate residents as leaders in radiation oncology involved in the future direction of cancer research by supporting investigator-initiated research and the Holman Pathway.
- The program should emphasize training Holman Pathway candidates, and clinicians to serve the state of Iowa and the Midwest.
- Continue to seek out exceptional residents who show qualities of empathy, dedication to the field, excellent communication skills, professionalism, and self-motivation. Promote the development of sound clinical skills and medical knowledge.
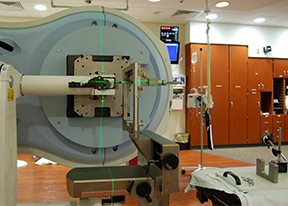
Facilities
Radiation Oncology Center for Excellence
Since moving to our present location in 2008, the Center for Excellence in Image Guided Radiation Therapy has provided exceptional care to patients seen in our clinic. Through constant innovation we have provided our patients access to the best imaging modalities and state-of-the-art treatments.
Patients benefit from being imaged on a 3T MRI, PET-CT and cone-beam CT before treatment. State-of-the-art treatments and devices including IORT, SBRT, HDR-brachytherapy, 4-D gating, TSE therapy, and MR-Linac complement the more traditional treatments available using linear accelerators.
Our staff are devoted to the patients they care for, which is evident in the highest patient satisfaction ratings within the hospital unit. Each is committed to improving patient care through education, research and a "patient-first" ethos.
- Learn more about the Radiation Oncology Center for Excellence.
Holden Comprehensive Cancer Center
The Holden Comprehensive Cancer Center is the only National Cancer Institute (NCI) accredited cancer center in the state of Iowa designated as "comprehensive". This is a five-year designation (2021). A truly interdisciplinary Clinic means that patients may be seen by physicians of several specialties during the same appointment. The space occupied by the Clinic includes a pharmacy and a laboratory as well as ample provision for families accompanying their loved ones to treatment.
- Learn more about the Holden Comprehensive Cancer Center.
Quick Facts
- A varying number of residents are accepted each year depending on the number of positions available
- 7 total residents are ACGME approved for our training program
- Graduates are well prepared to work in academic institutions and/or community practices
- Over 25 departmental faculty members (including Radiation Oncology physicians, Medical Physicists, and Free Radical and Radiation Biologists) train and mentor our radiation oncology residents
Scheduling/Rotations
- Residents rotate several times with each physician faculty in specialized clinics ensuring that the breadth and depth of each disease site is covered
- Research rotations in the first and second year give residents dedicated time and resources to actively engage in research and produce/submit abstracts and manuscripts
- Pathways (16 weeks) allow for PGY4-5 residents to individualize their residency education and specialize in areas of interest within the field.
FAQs
What procedures do you do in your clinic?
 We have incredibly strong physics support, which allows us to do a wide variety of special procedures such as: low dose rate brachytherapy for prostate cancer, high dose rate brachytherapy for gynecologic cancers, intraoperative radiation therapy for breast cancer, stereotactic radiosurgery for intracranial lesions, frameless stereotactic radiotherapy, stereotactic body radiosurgery for liver and lung tumors, gated treatment delivery, conebeam CT for tumor localization, total body radiation therapy, and total skin radiation therapy.
We have incredibly strong physics support, which allows us to do a wide variety of special procedures such as: low dose rate brachytherapy for prostate cancer, high dose rate brachytherapy for gynecologic cancers, intraoperative radiation therapy for breast cancer, stereotactic radiosurgery for intracranial lesions, frameless stereotactic radiotherapy, stereotactic body radiosurgery for liver and lung tumors, gated treatment delivery, conebeam CT for tumor localization, total body radiation therapy, and total skin radiation therapy.
Is there sufficient patient volume so that I can have multiple exposures to a variety of conditions?
- One of the strengths of our residency program is that we see a wide variety of cases. We are fortunate to work in an excellent hospital with strong programs in multiple disciplines, such as Otolaryngology, Neurosurgery, and Medical Oncology to name a few. These departments see patients from all over Eastern Iowa, and those patients are then subsequently referred to our department for radiation therapy. We typically have 60 – 90 patients under treatment at any time.
Do I have to rotate outside UI Hospitals & Clinics to fulfill requirements?
- There are enough brachytherapy and pediatric cases to fulfill requirements for board certification. If residents are interested in additional experience in these areas, outside rotations can be arranged.
What's the call schedule like?
- Residents take call several times throughout the year for 1 week. Occasionally, residents are needed to cover the clinic briefly on Saturday or Sunday mornings. Rarely, residents are called during the night to emergently treat a patient.
Do you have a research project requirement for graduation?
- Yes. Not only do we have a research project requirement, but we have a research curriculum in the first two years of residency that helps strengthen and promote research skills while giving residents dedicated time to focus on their projects. Our residents have been very successful and productive in their research efforts and have all been accepted to present a poster at our national specialty conference, ASTRO. Additionally, residents can choose a research pathway in their last two years if interested.
Are residents involved in any clinical trials/protocols?
 We encourage all residents to be involved in clinical trials. We try to tailor residency to a particular resident’s individual needs and interests. Residents who are interested in a career in academic Radiation Oncology will likely opt for our Research or Holman Pathways. Other residents interested in private practice will also have ongoing research projects, but will focus more on developing their expertise on our Clinical Pathway.
We encourage all residents to be involved in clinical trials. We try to tailor residency to a particular resident’s individual needs and interests. Residents who are interested in a career in academic Radiation Oncology will likely opt for our Research or Holman Pathways. Other residents interested in private practice will also have ongoing research projects, but will focus more on developing their expertise on our Clinical Pathway.
What's Iowa got that other programs don't?
- State-of-the-art technology
- Individualized, innovative and integrative curriculum
- Nationally and internationally recognized faculty leaders in the fields of Radiation Oncology, Medical Physics and Free Radical and Radiation Biology
- A dedicated Education Team as well as Clinical Research Team
- Iowa City is a highly intellectual community with premier arts events that are accessible to residents in terms of cost and location
- We have an outstanding school system for children in grades K-12
- A great training program and a high quality of life at an affordable price
- Great benefits
4-Year Educational Plan
 In order to train future practitioners of radiation oncology, we provide a comprehensive educational experience that will expose residents to all aspects of radiation oncology. We have designed a curriculum that is innovative, individualized and integrative. The residency experience entails clinical rotations, didactics (graduate level courses and several weekly conferences and tumor boards) dedicated research time, and pathways that allow residents to specialize and focus on areas of interest within the specialty. Residents finish the program with a deep understanding of cancer including the biology, pathology, natural history, work-up and treatment approaches with radiation therapy, surgery and chemotherapy. Residents become competent in the delivery of radiation therapy including techniques of external beam radiotherapy as well as interstitial and intracavitary radiotherapy. Through a variety of experiences and resources available, residents become well prepared for their board examinations.
In order to train future practitioners of radiation oncology, we provide a comprehensive educational experience that will expose residents to all aspects of radiation oncology. We have designed a curriculum that is innovative, individualized and integrative. The residency experience entails clinical rotations, didactics (graduate level courses and several weekly conferences and tumor boards) dedicated research time, and pathways that allow residents to specialize and focus on areas of interest within the specialty. Residents finish the program with a deep understanding of cancer including the biology, pathology, natural history, work-up and treatment approaches with radiation therapy, surgery and chemotherapy. Residents become competent in the delivery of radiation therapy including techniques of external beam radiotherapy as well as interstitial and intracavitary radiotherapy. Through a variety of experiences and resources available, residents become well prepared for their board examinations.
Clinical Rotations
Radiation Oncology Clinical Service
In order to obtain the essential skills and knowledge, residents will spend a significant portion of their residency on the Radiation Oncology Clinical Services. Each physician faculty runs their own clinical service specializing in specific disease sites. Residents will rotate through each service at least three times throughout residency and potentially more if interested in a specific service/disease. Clinical rotations will vary in length each training year in order to meet the overall educational learning goals.
Department faculty clinical services include:
| Faculty Clinical Service | Topics/Disease Sites | Special Procedures |
|---|---|---|
| Carryn Anderson, MD | Head and Neck, Melanoma, Sarcoma, Skin/Soft Tissues | Eye Plaque Brachytherapy, Spinal Stereotactic Radiosurgery |
| John Buatti, MD | Pediatrics, Head and Neck, Skin, Central Nervous System | Extracranial Stereotactic Radiosurgery, Craniospinal Stereotactic Radiosurgery, Radiation Therapy, and Eye Plaque Brachytherapy |
| Bryan Allen, MD | Thoracic Cavity, Lung | Thoracic Malignancies, Eye Plaque Brachytherapy, Pancreatic/Esophageal Stereotactic Radiosurgery |
| Mark Smith, MD | Brain, Central Nervous System, Genitourinary, Lymphomas and Leukemias, Palliation | Prostate Stereotactic Radiosurgery, Brachytherapy, Cardiospinal Radiation, Total Body Irradiation Therapy, and Eye Plaque Brachytherapy |
| Wenqing Sun, MD | Gynecology, Breast, Head and Neck | Gynecologic Brachytherapy, Breast Brachytherapy, and Eye Plaque Brachytherapy |
| Joseph Caster, MD, PhD | Gastrointestinal, Gynecologic | Eye Plaque and Gynecologic Brachytherapy, Prostate Stereotactic Radiosurgery, Pancreatic/Esophageal Stereotactic Radiosurgery |
| Kristin Plichta, MD, PhD | Thoracic Cavity, Breast | Breast and Eye Plaque Brachytherapy and Thoracic Malignancies |
Selectives
These blocks are additional clinical experiences that further enhance the understanding of Radiation Oncology.
- Radiology - An optional four-week rotation that consists of a combined experience in Diagnostic Radiology, PET/Nuclear Medicine and Neuroradiology taken in PGY3
- Dosimetry - A designated 4-week block that focuses on the clinical integration of Radiation Oncology taken in PGY2
Clinical Experience Overview
Learning Goals:
- PGY2: Foundation and Exposure
- PGY3 - PGY4: In-depth Understanding/Learning, Increase Responsibility
- PGY5: Specialize/Focus and Autonomy
| PGY2 | PGY3 | PGY4 | PGY5 | Total Weeks | ||
|---|---|---|---|---|---|---|
| Clinical Radiation Oncology (Faculty Services) | 44 weeks 5-6 8-week blocks Exposure to all clinics |
40 weeks 5 8-week blocks Increase depth of clinical understanding |
44 weeks 5-6 8-week blocks Repeat area of interest |
36 weeks 5 8-week blocks Resident choice of clinic based on career path |
164 weeks | |
| Selectives | 4 weeks Dosimetry |
4 weeks optional Radiology |
4 weeks optional Radiology |
8 weeks |
Conferences
Both conferences and courses are offered on a continual basis that residents are required to attend in order to be exposed to the full spectrum of content in Radiation Oncology.
Residents have the opportunity to learn from faculty, guest speakers, and peers in a myriad of venues, including several departmental as well as interdisciplinary conferences and tumor boards on a weekly basis. Residents also develop excellent presentation and speaking skills by frequently giving lectures and honing their teaching efforts.
Clinical Case Conferences
Twice a week, residents and faculty present Case Conferences that pertain to specified disease sites and relevant patient cases. Residents present ½ hour, concise power point presentations on a disease site, while faculty facilitate discussion and present patient cases to engage all learners in this interactive learning session. Both residents and faculty come prepared to teach and learn! Topics are presented in a longitudinal curricular approach so residents are exposed to all topics throughout the year rather than one month at a time.
The following elements are included in each Case Conference pertaining to the disease site:
- Work up, diagnosis and staging of the patient’s case
- Treatment options
- Particular radiation plan used to treat the patient
- Review of relevant sentinel studies or literature supporting the use of radiation for the patient
- Potential acute and long-term complications of the treatment
- Prognosis and other expected outcomes
- Relevant patient cases
Chart Rounds
Chart Rounds occur once a week and focus on our clinic patients starting treatment. Residents briefly present the patient’s diagnosis, stage, brief history, and a description of the treatment plan. Input is provided from faculty, physicists, dosimetrists, and staff.
Residents become very familiar with the patient’s treatment plan by displaying and describing relevant treatment fields and dosimetry, understanding how the GTVs, CTVs, and PTVs were constructed, and awareness of the goal doses to each PTV along with the doses to each dose-limiting structure.
Journal Club
Journal Club meets at least six times a year to focus on Practice-Based Learning and Improvement skills. The curriculum prepares residents to effectively investigate and evaluate their patient care practices, and appraise/ assimilate scientific evidence by utilizing an Evidence Based Medicine approach. Residents will increase their EBM skills, effectively be able to facilitate a Journal Club discussion and ultimately apply their knowledge to improve their own patient care.
Tumor Boards
Residents are required to attend specific disease-site Tumor Boards. Medical and allied professionals from a variety of departments attend tumor board conferences and focus on the interdisciplinary nature of patient care. The following Tumor Boards are scheduled 2-4 times a month.
- Melanoma
- Thoracic
- Sarcoma
- Lymphoma
- Gyn Onc
- Peds Onc
- Neuro-Path
- Genitourinary
- Head and Neck
- Breast
- Hepatic
Personal and Professional Development Series
To help residents grow personally, professionally, and healthfully, the Department offers this series to cover a variety of issues relevant to a resident’s life, practice and health. Residents meet with a variety of in-house guest speakers and discuss topics listed below. Additionally, every year the department sponsors a Resident Retreat that focuses on resident wellness, team building and special topic issues.
- Giving Bad News
- Nursing Topics
- Impaired Residents/Faculty
- Billing and Coding
- Teaching Skills
- Cultural Diversity
- Pain Management
- Interviewing/CVs
- Stress Management
- Palliative Care and Hospice
- Ethics
- Finances
- Leadership Skills
Courses
The residency curriculum includes teaching of basic sciences essential to training in radiation oncology, including radiation biology and Medical Physics. These courses are taught by our own medical physics and Free Radical and Radiation Biology faculty. Residents are relieved of all clinical duties during course meeting times. Courses are required and taken the first two years of residency. PGY4 and PGY5 residents have the option of repeating the courses to further their understanding and learning. Departmental courses offered include:
| Course | Students | Offered |
|---|---|---|
| Medical Physics* | RTT Students Rad Onc Residents FRRB Graduate Students Dental Residents/Fellows |
Every Spring and Fall Semester |
| Radiation Biology* | Rad Onc Residents FRRB Graduate Students Other Graduate Students |
Fall Semester, Odd Years |
| Biostatistics | Rad Onc Residents | Spring Semester, Even Years |
* Graduate level course
Independent Study and Board Preparation
 The field of Radiation Oncology is a highly academic specialty in which residents need to continually and consistently on their own, study the vast amount of content. For successful completion of the residency program, passing boards and effectively integrating knowledge into patient care – it is expected that each resident begins this independent study process from day one of residency. Residents will develop their own Learning Plan each year and will be monitored for progress by the Program Director semi-annually.
The field of Radiation Oncology is a highly academic specialty in which residents need to continually and consistently on their own, study the vast amount of content. For successful completion of the residency program, passing boards and effectively integrating knowledge into patient care – it is expected that each resident begins this independent study process from day one of residency. Residents will develop their own Learning Plan each year and will be monitored for progress by the Program Director semi-annually.
In addition to independent study, the program offers several exams annually to help prepare residents for boards. Residents are required to take and perform at an expected level for the following exams: In-Service, RAPHEX (physics), and Mock Orals. In-Service and RAPHEX exam scores allow residents to compare and gauge their performance nationally against their peers. The goal of mock oral exams is to simulate the actual board exam so residents are not only prepared for the medical knowledge but for the test-taking skill itself. Residents also have the opportunity to take the RABEX (radiation biology).
Research
Research is a vital component of the residency program. A curriculum has been established to hone resident research skills and knowledge with ample research opportunities and resources while providing residents with dedicated, protected time for their clinical research. The department has a research team that serves as mentors and resources for residents. Protected research time is tailored to resident needs and interests and is most often arranged during PGY3-PGY5. Every resident is expected to have submitted a manuscript for publication by the end of residency.
 Resident Research
Resident Research
Residents in our department have been very productive and successful with their research endeavors. Each resident has one or more abstract acceptances to national conferences and many have manuscript submissions.
Resident Research Showcase
We are very proud of our resident research efforts, and want to showcase their projects! The Annual Resident Research Showcase is held during the annual ISTRO meeting. This allows residents to present their posters to meeting participants while also giving them experience and feedback on their presentation and poster before they present at ASTRO.
PGY4-5 Research Opportunities
Some residents choose to continue their research endeavors more in-depth. Residents can select to do a Clinical Research Pathway or apply for the Holman Pathway for those who want a career as a physician investigator and are interested in basic science, clinical or translational research.
Pathways
“The beauty of our clinical pathways, whether it be academics, research, or community medicine, is that they allow us to be well-rounded, competent clinicians while providing us the autonomy and initiative to fashion our unique niches in health care (medical education, innovation, public policy, global health, clinical trial initiation, etc.)."
-Sagar C. Patel, MD
In order to help residents meet the learning goal of focusing and specializing in areas of interest, residents will choose and/or develop a Pathway by mid-residency. Pathways are individualized learning experiences developed around specific areas that correlate to each resident’s personal career goals and interests. Approximately 16 weeks of residency will be devoted to a selected Pathway to be taken in PGY4 and PGY5. Currently, developed Pathways include, but certainly are not limited to:
- Clinical Research - Residents who develop a keen interest in clinical research after the first two years can continue their projects and further develop their skills
- Academic Medicine - Residents interested in pursuing an academic career i.e., in medical education, public health, etc. can work simultaneously on their Masters degrees in Medical Education or Public Health during residency.
- Clinical Medicine - Residents who want to focus more on their clinical skills and practice can choose the Clinical Medicine Pathway. Learning experiences will encompass more exposure and experience for specific procedures or disease sites and a variety of clinical Radiation Oncology experiences (i.e. community medicine rotations)
The Holman Pathway
“The Holman Pathway afforded me protected time to really focus on basic science research and provided me a foundation for a successful academic career as a physician-scientist.”
–Darrion Mitchell, MD, PhD
The Holman Pathway presents an alternative residency structure for selected residents in Radiation Oncology. It’s a special training program available for residents who are planning a career in basic science or clinical research. Residents become eligible for board certification after 21 months of research and 27 months of clinical training.
Holman Pathway residents are required to meet the same minimum requirements for special procedures (interstitial and intracaviatry brachtherapy and unsealed sources) as well as pediatric cases. HP residents are not required to take the curriculum selectives (Radiology, Physics, and Dosimetry and the PGY3 Research Curriculum). Additionally, the clinical rotations will be designed to meet the HP resident needs.
Learn more about the Holman Pathway.
Program Accreditation & Board Certification
The radiation oncology residency at University of Iowa Hospitals & Clinics is accredited by the Accreditation Council for Graduate Medical Education. Our last ACGME site visit was January 2024. The program is approved for 7 total resident positions.
Information specific to program requirements for a radiation oncology training program may be found at the ACGME.
Please visit The American Board of Radiology website for board certification requirements.
How to Apply
Our four-year radiation oncology residency is available to those who have completed their first post-graduate year in internal medicine, family medicine, obstetrics and gynecology, surgery or surgical specialties, pediatrics, or a transitional year program, which must include at least nine months of direct patient care in medical and/or surgical specialties other than radiation oncology.
Our program will be accepting applications for 2 vacancies in ERAS season 2025.
Applications will be accepted through the Electronic Residency Application System (ERAS).
All applicants must also register with the National Resident Matching Program (NRMP). The NRMP number for our programs is: 1203430A0
International medical graduates should contact the ECFMG. An ECFMG certificate must accompany the ERAS application.
*Applicants are responsible for applying for a separate PGY-1 intern year in an ACGME-accredited program.
A complete ERAS application includes:
- Personal statement
- Medical Student Performance Evaluation (MSPE)
- Three letters of recommendation
- Passing USMLE scores
- Medical school transcript
- Recent photograph
- ECFMG status report, if applicable
Certification
American Board of Radiology Certification
The American Board of Radiology (ABR) conducts initial qualifying and certifying examinations to ascertain the qualification of those who have completed training in radiation oncology.
Information regarding ABR Certification may be viewed on the Board’s website
Contact
Thank you for your interest in our program. If you have any questions, please contact us.
Program Contact:
Rachel Kadlec
Residency Coordinator
rachel-kadlec@uiowa.edu
(319) 384-6135
Deadlines
Applications will be accepted through October 15 for PGY2 positions. Applicants are responsible for applying for transitional year residency separately.
Virtual Meet & Greet
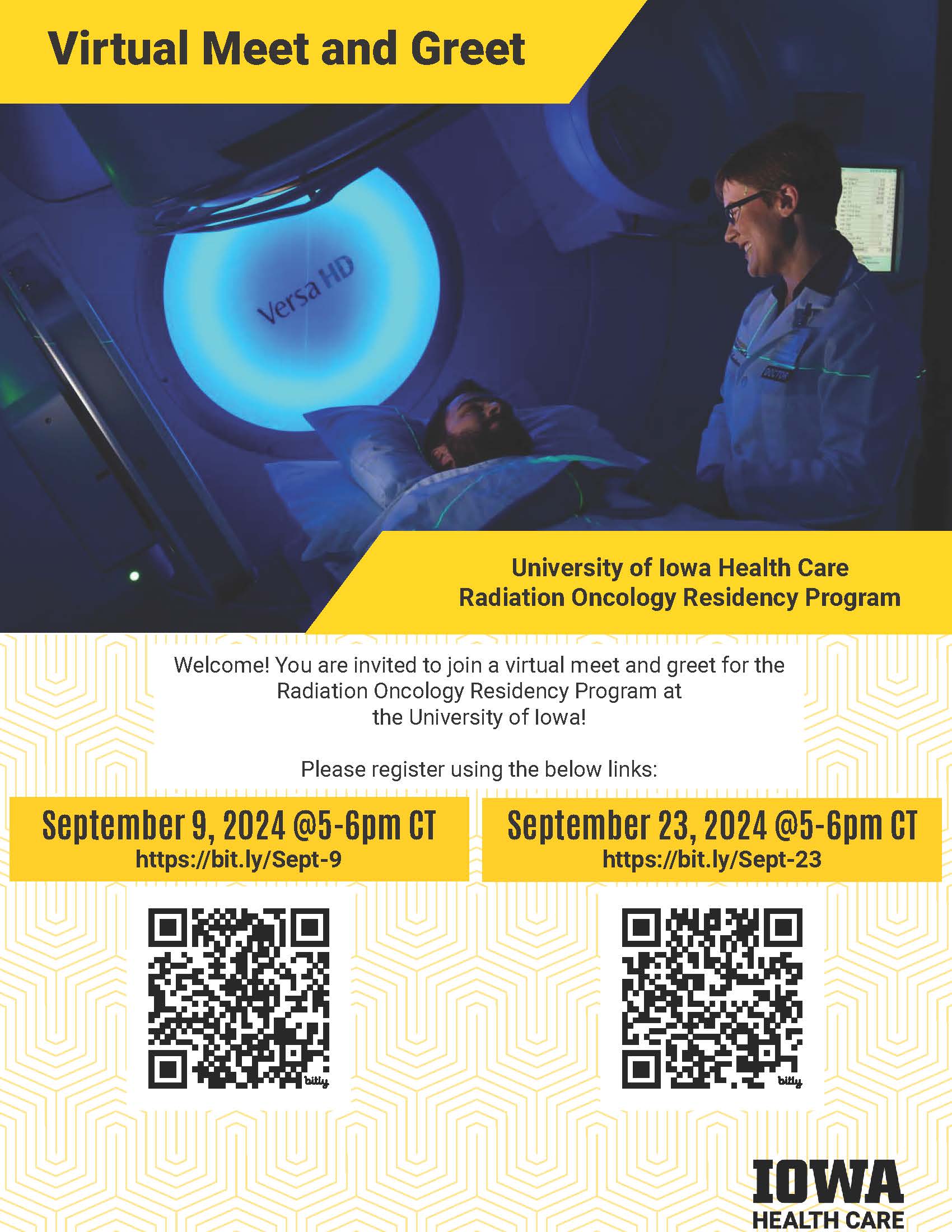
Couples Match
The Department of Radiation Oncology encourages couples match applications. If an applicant is selected to interview with us, we will work in conjunction with the corresponding department to attempt to streamline interview dates and times for both applications. More information on couples matching can be found on the NRMP website.
Criteria
It is the goal of the Department of Radiation Oncology at the University of Iowa to produce quality radiation oncologists who pursue either an academic or private practice career. To do this, we feel that it is necessary to choose high quality residents from the pool of applicants each year. Future residents are selected based on academic achievement, personal qualities, and the faculty's assessment of their potential to excel in the residency program. In general, most successful applicants are in the top third of their medical school class and graduate from LCGME schools that provide superior undergraduate medical education.
Interviews
Dates
Our program will be recruiting two PGY-2 positions in ERAS 2025 season. Selected candidates will be notified of selection for an interview via Thalamus. Interviews will take place from December through January.
Sample Interview Schedule
Candidates can anticipate the interview day to span from 8am (CST) until 2pm (CST)
The interview day will begin with a forty-minute Informational Presentation, led by Residency Program Director, Kristin Plichta, MD and Department Chair, Bryan Allen, MD commencing at roughly 8am (CST).
Following the introduction, candidates will have a short break, with an option to join a casual virtual waiting room.
Following breaks, interviews will commence in 20-minute panel style sessions composed of 2-3 faculty members in each treatment area (i.e., Head & Neck, Pediatrics, Breast, Gynecology, etc.), as well as individuals from our Med Physics team and Free Radical/Rad Biology teams.
Candidates will have 10 minutes to break in-between sessions (again, with an option to join the virtual waiting room).
All candidates will have a casual meeting with current residents over the lunch hour and commence with additional afternoon interview sessions
The interview day will end with a 30-minute Meet and Greet session with our Free Radical/Rad Biology Team, which will include information regarding research opportunities
Our People
Our department is patient centered and the attitude shared by staff reflects this. Faculty compose a good blend of clinical and research skill sets with a broad knowledge of all the treatment modalities, yet with a profound depth of knowledge in their specialty area.
Many of the clinical-track graduating physicians begin careers in private practice with the balance entering academic medicine.
Each of our Faculty members is board certified in Radiation Therapy and accredited. Owing to the interdisciplinary nature of Radiation Therapy many share joint appointments in other disciplines.
Welcome From the Residency Program Director
Welcome From the Residency Program Director
On behalf of the University of Iowa Department of Radiation Oncology, I would like to personally invite you to explore our Department and Residency Program. Education is a key component of our mission, and we are committed to providing residents with an outstanding educational experience.
Our residency program has many features that distinguish it from other programs. Residents receive training not only from nationally recognized radiation oncologists but also free-radical radiation biologists and medical physicists. As the only academic radiation oncology program in our region, we draw patients from Iowa and beyond. You will treat diverse diseases and people, and our residents do not need to take “away rotations” to satisfy pediatric or brachytherapy rotations. Our department prides itself on our state-of-the-art technology utilized in the clinic and hospital, allowing for up-to-date training and preparation for independent practice. Technologies include CT, PET and MR simulation imaging within the department, an Elekta Unity MR-Linac, a Leksell Gamma Knife Icon, and a joint Theranostics clinic with Nuclear Medicine.
One of the most unique and innovative features of our curriculum is our residency pathways. These pathways allow residents to specialize and focus on areas of interest within the field of radiation oncology, such as clinical medicine, academic medicine and research. In additional to our pathways, residents also rotate on clinical services, have dedicated research time, take courses in Medical Physics, Radiation Biology and Biostatics, and participate in didactic case conferences designed to fully prepare them for independent practice in academic medicine or private practice. The residency is accredited by the Accreditation Council for Graduate Medical Education, and we currently have seven residents.
Please peruse our website to learn more about our program, where you will find detailed information regarding our curriculum including clinical experiences, didactics, and research opportunities. If you have any questions, please email me or any other faculty and staff in the department.
Clinical Assistant Professor, Department of Radiation Oncology
Program Director, Department of Radiation Oncology
Current Residents
Class of 2026
Shri Kiriti Rajan, MD
Transitional Year: University of Texas Southwestern - Dallas, TX
MD - University of Alabama School of Medicine - Birmingham, AL
Uwajah Uzomah, MD
Transitional Year: Piedmont Athens Regional Medical Center - Athens, GA
MD - University of Ibadan College of Medicine - Ibadan, Oyo State, Nigeria
MPH - Harvard Chan School of Public Health, Harvard University - Boston, MA
Class of 2027
Moses Evbuomwan, MD
Transitional Year: Campbell University - Buies Creek, NC
MD - Oakland University William Beaumont School Of Medicine - Auburn Hills, MI
MPH - University of Miami - Coral Gables, FL
Ashley Way, MD
Transitional Year: Baylor College of Medicine - Houston, TX
MD - Ross University School of Medicine - Bridgetown, Barbados
MPH - Chamberlain University - Downers Grove, IL
Class of 2028
Olukemi Alegi, MD
Transitional Year: Piedmont Athens Regional Medical Center - Athens, GA
MBChB - Kwame Nkrumah University of Science & Technology - Kumasi, Ghana
Matthew Roozeboom, DO
Transitional Year: Medical College of Wisconsin Affiliated Hospitals - Milwaukee, WI
DO - Des Moines University College of Osteopathic Medicine - Des Moines, IA
Alumni Residents
| Graduated | Resident | Last Known Employment |
|---|---|---|
| 2024 | Breann Bowar, MD | Radiation Oncologist, University of Nebraska Medical Center, Omaha, Nebraska |
| 2024 | Qateeb Khan, MD | Assistant Professor, University of Nebraska Medical Center, Omaha, Nebraska |
| 2023 | Jordan Gainey, MD | Radiation Oncologist, Palmetto Radiation Oncology, Florence, South Carolina |
| 2023 | Calvin Lewis, MD, PhD | Radiation Oncologist, Colorado Urology Prostate Cancer Center, Greenwood Village, Colorado |
| 2023 | Jonathan Van Wickle, MD | Radiation Oncologist, Coastal Radiation Oncology, Mission Hope Cancer Center, Santa Maria, California |
| 2022 | Quentin Adams, MD | Radiation Oncologist, Pineville Radiation Therapy Center, Charlotte, North Carolina |
| 2022 | Cameron Callaghan, MD, MPH | Radiation Oncologist, Mayo Clinic, Rochester, Minnesota |
| 2020 | Steven Seyedin, MD | Assistant Clinical Professor, University of California, Irvine-Chao Family Comprehensive Cancer Center, Orange, California |
| 2020 | Addison Willett, MD, JD | Radiation Oncologist, Mobile Infirmary Cancer Center, Mobile, Alabama |
| 2019 | Michael Marquardt, MD, MPH | Radiation Oncologist, Mercy Medical Hall-Perrine Cancer Center, Cedar Rapids, Iowa |
| 2019 | Imran Mohiuddin, MD, PhD | Radiation Oncologist, AdventHealth, Orlando, Florida |
| 2019 | Jessica Parkhurst, MD | Clinical Assistant Professor, University of Iowa Hospitals & Clinics, Holden Comprehensive Cancer Center, Iowa City, Iowa |
| 2018 | Kristin Plichta, MD, PhD | Assistant Professor, University of Iowa Hospitals & Clinics, Department of Radiation Oncology, Iowa City, Iowa |
| 2018 | Amir Zahra, DO | Radiation Oncologist, Nebraska Cancer Specialists, Omaha, Nebraska |
| 2016 | Darrion Mitchell MD, PhD | Assistant Professor, The Ohio State University Wexner Medical Center, Department of Radiation Oncology, Columbus, Ohio |
| 2016 | Sagar Patel, MD | Radiation Oncologist, Cape Radiation Oncology, Cape Girardeau, Missouri |
| 2015 | Andrew Hoover, MD | Associate Professor, University of Kansas Medical Center, Department of Radiation Oncology, Kansas City, Kansas |
| 2015 | Hualei Li, MD, PhD | Radiation Oncologist, Indiana University Health, Martinsville, Indiana |
| 2014 | Ann Morris, MD | Radiation Oncologist, University of Kansas Cancer Center, Overland Park, Kansas |
| 2014 | Arshin Sheybani, MD | Radiation Oncologist, John Stoddard Cancer Center, Des Moines, Iowa |
| 2013 | Bryan Allen, MD, PhD | Associate Professor, University of Iowa Hospitals & Clinics, Department of Radiation Oncology, Iowa City, Iowa |
| 2012 | Charles Murphy, MD | Clinical Associate Professor, USD Sanford School of Medicine, Avera Radiation Oncology, Sioux Falls, South Dakota |
| 2012 | Bill Rockey, MD | Associate Professor, University of Iowa Hospitals & Clinics, Department of Radiation Oncology, Iowa City, Iowa |
| 2011 | Joni Buechler-Price, MD | Radiation Oncologist, Prairie Lakes Healthcare System, Watertown, South Dakota |
| 2011 | Wenqing Sun, MD | Associate Professor, University of Iowa Hospitals & Clinics, Department of Radiation Oncology, Iowa City, Iowa |
| 2010 | Samuel Andrews, MD | Radiation Oncologist, University of Iowa Hospitals & Clinics, Iowa City, Iowa |
| 2010 | Anna Olson, MD | Radiation Oncologist, Mayo Clinic Health System, La Crosse, Wisconsin |
| 2009 | Casey Duncan, MD | Radiation Oncologist, Cancer Care Specialists of Illinois, Effingham, Illinois |
| 2008 | David Mattson, MD, PhD | Associate Professor, Department of Radiation Medicine and Director, GI & GYN Radiation Oncology, Roswell Park Cancer Center Institute, State University of New York, Buffalo, New York |
| 2007 | Joel Simmons, MD | Radiation Oncologist, Kettering Cancer Care, Kettering, Ohio |
Radiation Oncology Faculty Listing
Redirected to CCOM faculty listing page. Keep so the menu link works on the book.
https://hc-vbugtracker.healthcare.uiowa.edu//issues/8320
Renamed to "Radiation Oncology Faculty Listing and redirected:
https://gme.medicine.uiowa.edu/radiation-oncology-residency/our-people/m...
Update can be reviewed from:
https://gme.medicine.uiowa.edu/radiation-oncology-residency/our-people
Free Radical and Radiation Biology Faculty
The University of Iowa is the only institution in the USA to offer a graduate degree in Free Radical and Radiation Biology FRRBP within a clinical department. Emphasizing the multi-disciplinary nature of the program, students have access to 7 primary and 21 adjunct faculty covering a wide gamut of scientific endeavor. One of the central purposes of the FRRBP is to study the effects of radio response of cancer cells in order to improve the treatment of cancer.
Learn more about the Free Radical and Radiation Biology Program and faculty.
Faculty Members
Kristin Plichta, MD, PhD
Residency Program Director, Clinical Assistant Professor of Radiation Oncology
Bryan Allen, MBA, MD, PhD
Professor, Chair and DEO of Radiation Oncology

Carryn Anderson, MD
Clinical Professor of Radiation Oncology

John Buatti, MD
Professor of Radiation Oncology
James Byrne, MD, PhD
Assistant Professor of Radiation Oncology
Joseph Caster, MD, PhD
Associate Professor of Radiation Oncology

Yousef Ismael, MD
Clinical Assistant Professor of Radiation Oncology - Ottumwa Partner Site
Sami Koro, MD
Clinical Assistant Professor of Radiation Oncology - Clinton Partner Site
William Rockey, MD, PHD
Clinical Associate Professor of Radiation Oncology - Burlington Partner Site

Mark Smith, MD
Clinical Professor of Radiation Oncology
Wenqing Sun, MD, PhD
Clinical Associate Professor of Radiation Oncology
Kailin Yang, MD, PhD
Clinical Assistant Professor of Radiation Oncology
Contact Us
The Department of Radiation Oncology is committed to education and the development of the next generation of leaders in our field. To help accomplish our educational goals, continually improve and deliver the best residency education, a Residency Education Team has been created. Each member on this team has a complement area of expertise in graduate medical education.
Kristin Plichta, MD, PhD
Program Director
kristin-plichta@uiowa.edu
Rachel Kadlec, MSL
Residency Coordinator
rachel-kadlec@uiowa.edu