Innovations
Teaching Skills Curriculum
In addition to a three-year, rolling curriculum, our program also offers a dedicated teaching rotation in the third year, as well as more advanced training.
Ultrasound Curriculum
Our longitudinal training in point-of-care ultrasound (POCUS) results in residency graduates with skills that would normally only be obtained in radiology or emergency medicine programs.
Quality & Safety Curriculum
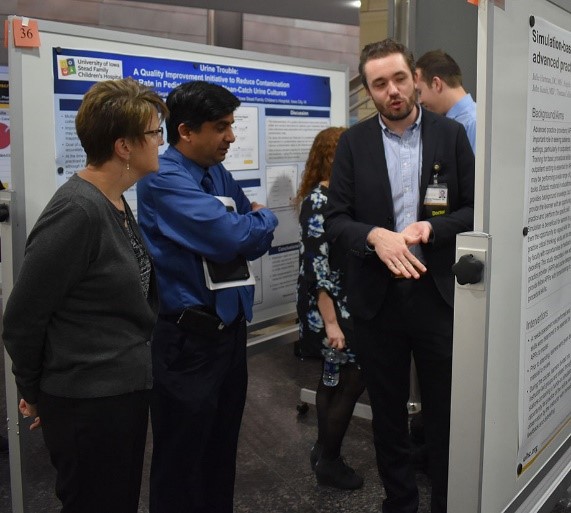
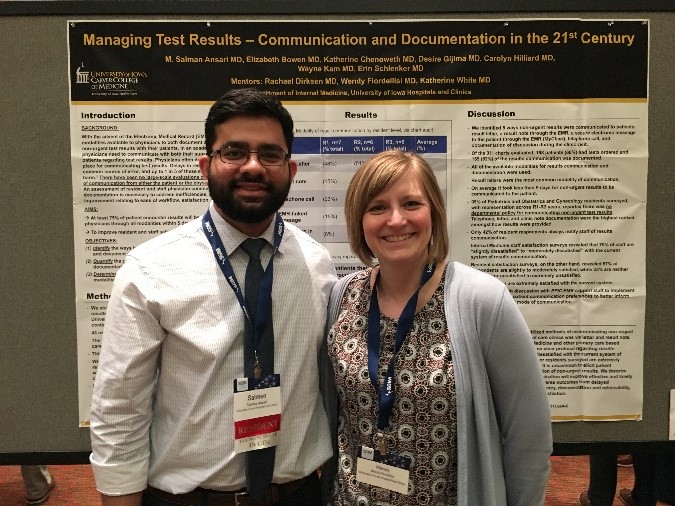
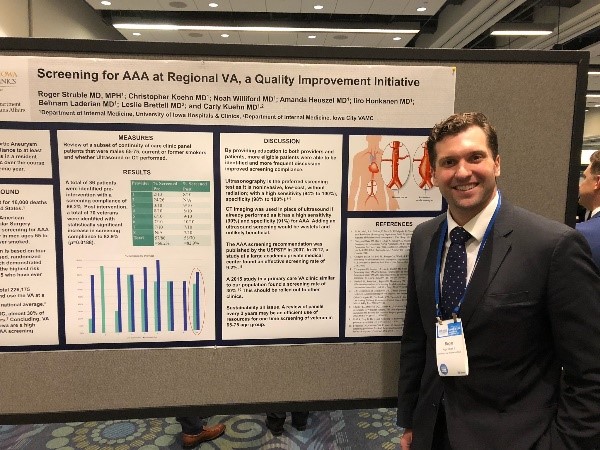
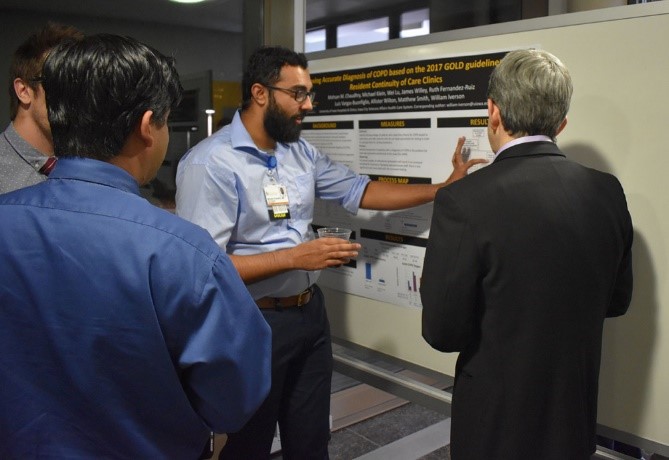
Quality improvement benefits our patients and our systems, but it also provides our residents with an opportunity to lead a focused project often resulting in a publication or presentation at a regional or national society meeting. We have carved-out protected time for this work and our VA-funded Chief Resident for Quality & Safety is just one of the mentors guiding residents.
qUIkCoach
Through the department, we have been able to develop an app available for our residents called qUIkcoach. This is a new app that is able to request and provide just-in-time feedback on a variety of different skills including clinical reasoning, communication, oral presentation, and notes. This allows for more directed feedback with a quicker turnaround time.
Ultrasound Curriculum
Point of Care Ultrasound Curriculum Overview
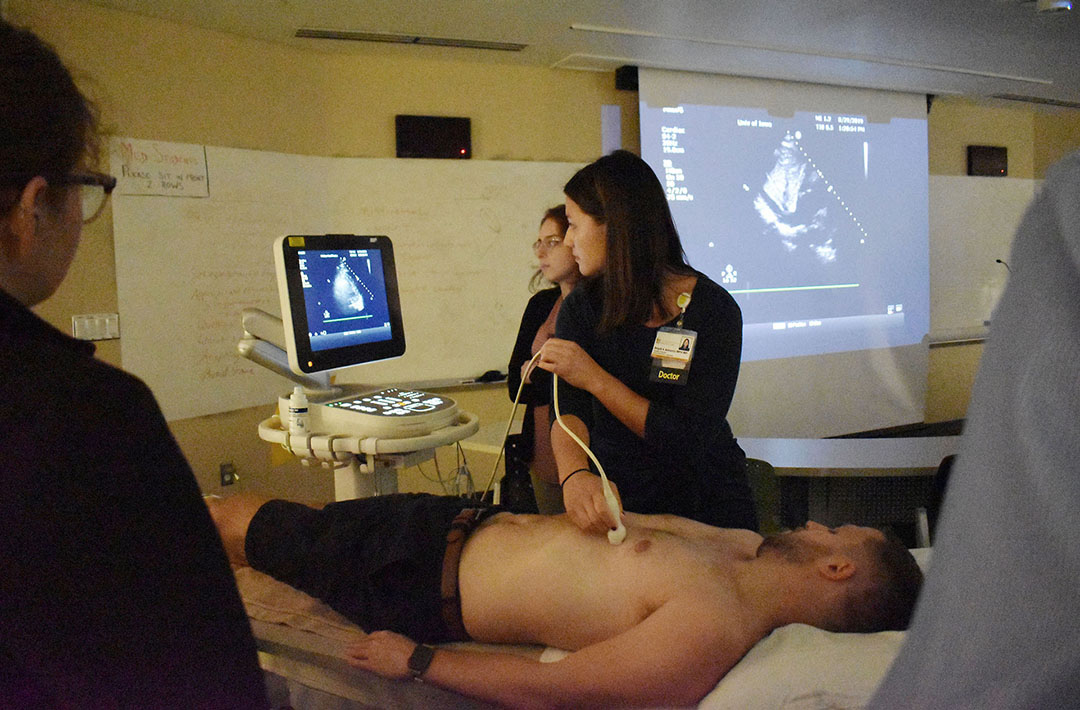
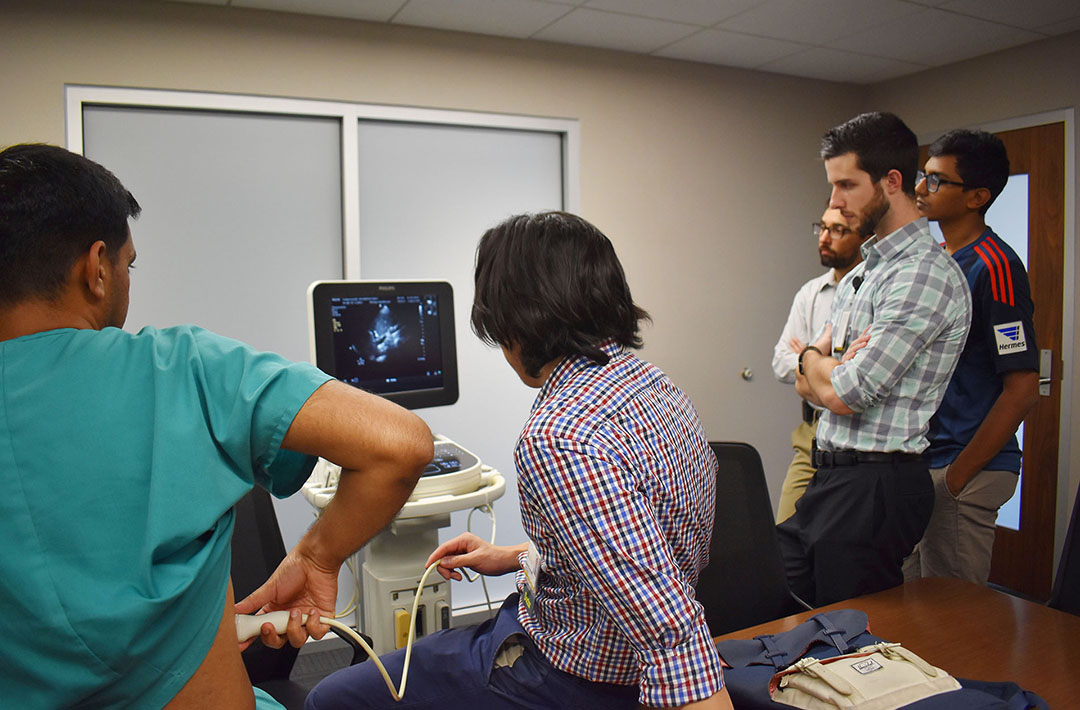
The University of Iowa Internal Medicine Residency Program Point-of-Care Ultrasound (POCUS) Curriculum is a longitudinal, integrated, and progressive learning experience. The POCUS curriculum is focused on teaching basic bedside ultrasonography and how it is utilized and applied to patient care in clinical internal medicine. The curriculum is integrated into and taught longitudinally during the academic half day during each resident’s ambulatory week (y-week). POCUS instruction is delivered by experienced faculty members, critical care fellows, and chief residents. POCUS skills assessments are completed for residents during each year of their training and the POCUS curriculum is modified on a yearly basis to best adapt to the needs of the trainees.
Curriculum Goal: At the end of the longitudinal POCUS curriculum, the resident will be able to acquire, interpret, and apply focused cardiac, lung, pleural, abdominal, and vascular ultrasound imaging into their clinical reasoning and medical decision making.
Teaching Methods:
- Independent pre-workshop learning materials (POCUS textbook chapters, online modules, etc)
- Short didactic sessions
- Hands-on scanning of simulated patients with live faculty mentors and real-time feedback
- Pathological image interpretation sessions
- Interactive ultrasound case studies
Modules:
| Basic POCUS Modules (PGY-1) | Advanced POCUS Modules (PGY-2 and above) |
|
|
Assessment: Pre- and post-curriculum assessment is completed annually to assess each individual trainee’s skills and knowledge acquisition and retention. These yearly assessments are also used to assess the curriculum and guide ongoing improvements in the POCUS curriculum. Assessment is completed using live ultrasound skills testing with faculty proctors, an electronic ultrasound knowledge assessment, and a resident survey.


Quality Improvement Curriculum
![]()
Check out the
QI information on our blog
Resident Quality Improvement Curriculum
The Internal Medicine Residency Program at the University of Iowa is committed to engaging residents in team-based Patient Safety/Quality Improvement projects to develop their knowledge and skills. It is our goal for every resident to be empowered to impact the quality and safety of their patients’ care during their residency and in their future careers. Our ground breaking curriculum was published in the Journal of Graduate Medical Education.
Objectives
- Actively and meaningfully participate in a team quality improvement project
- Work effectively with inter-professional teams on continuous quality improvement
- Apply continuous quality improvement to patient care
- Disseminate work in scholarly format
- Make a difference in the safety and quality of care of our current and future patients
Meet our Quality Improvement Leaders

Carly Kuehn, MD
Educational Director - Safety and Quality
Clinical Professor of Internal Medicine

Samuel Zetumer, MD
Chief Resident of Quality and Safety
Iowa City VA Medical Center
Quality Improvement Scholarship
The University of Iowa Department of Medicine understands that Quality Improvement and Patient Safety presents a phenomenal opportunity for scholarship for our residents. To showcase our commitment to our patient’s safety and to provide an avenue for scholarship the University of Iowa Hospitals and Clinics host an annual Quality and Safety Symposium in which our resident teams are given the opportunity, encouragement, resources, and mentorship to submit and present their projects. After this, many teams submit their projects to large regional and national meetings.
Since the development of our curriculum we have had…
- 50+ resident led QI Projects
- 30+ resident led QI Projects presented at our local Quality and Safety Symposium
- 25 resident teams present oral presentations or posters at SGIM Midwest Regional Meeting
- 7 resident teams present posters at SGIM National Meeting
- 2 resident teams present at Medicine or Psychiatry Conferences
Resident Quotes
“I felt as though I was making a quality change to improve the outpatient experience.”
“The QI curriculum gave us an opportunity for ownership over real positive change for our patients.”
“I actually know now the basics of how to design, implement, and interpret the results of a quality improvement project, which I didn’t know before.”