Teaching Skills Curriculum
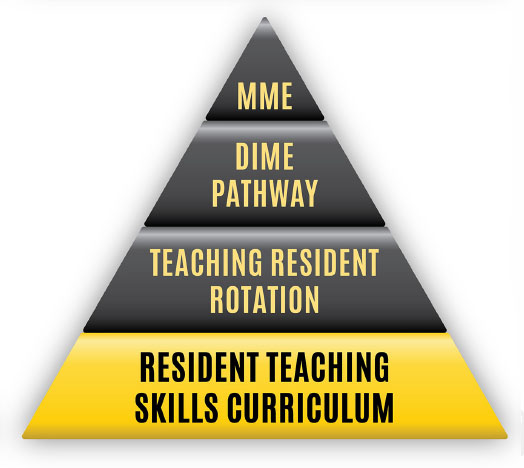
The Teaching Skills Curriculum is a longitudinal, integrated, and progressive workshop-based curriculum that introduces residents to the knowledge base and skill set used when serving in the role of a clinician-educator. This curriculum is taught during the academic half day of the Y-week. This curriculum focuses on skills and techniques that would be used to teach medical students while on rotations like creating an effective learning climate, one-minute preceptorship, and chalk-talk 101.

Teaching Skills Curriculum goals
The goal of the Teaching Skills curriculum is to introduce residents to a knowledge base and skill set used when serving in the role of a clinical educator. The longitudinal curriculum for all residents presents concepts and allows residents to practice skills associated with topics such as establishing the learning climate, motivating the learner, one-minute preceptor and feedback and evaluation as well as interactive teaching and evaluation.
Sessions are interactive covering a topic related to current best teaching practices. There is time for skill development and through the process of deliberate practice, residents design an action plan for further skill development. Residents complete pre-session readings and following each session are expected to refer to their action plan in teaching encounters.
Session #1: Introduction to Teaching Skills, Learning Climate and Effective Teachers
- identify characteristics of exemplary clinical teachers
- identify strategies to promote an effective learning climate
- demonstrate teaching behaviors that promote an effective learning climate
- develop an action plan to improve the learning climate in your own teaching
Session #2: Motivating the Learner
- examine contributing factors that affect a learner’s performance.
- explain one relevant motivational theory that covers extrinsic & intrinsic motivators.
- discuss the importance and impact of a good orientation.
- identify components of an orientation.
Session #3: One-Minute Preceptor
- describe the 5 elements of the one-minute preceptor model for clinical teaching.
- successfully apply the model to a simulated learner presenting a patient.
- use the model to develop an assessment of the learner’s current level of knowledge/skill and what the learner needs to know.
Session #4: Feedback
- define feedback and give rationale for providing feedback to learners.
- recognize barriers to giving feedback.
- identify characteristics of effective feedback.
- demonstrate effective feedback via observation and practice.
- develop an action plan for improving personal feedback skills.
Session #5: Interactive Teaching/Use of Technology
- know the goals of effective lecturing/presentation.
- describe components of effective lecturing/presentation.
- apply specific techniques for making lectures more interactive.
Session #6: Evaluation of Students, Peers and Faculty
- define evaluation and differentiate it from feedback.
- obtain an understanding of the use of commonly used evaluation tools and techniques.
- gain insight into common pitfalls surrounding evaluations.
- understand why accurate evaluation is important.