About the Program
Our division offers a three-year fellowship training program in the field of Pediatric Gastroenterology, Hepatology and Nutrition. The program has been fully accredited by the Residency Review Committee of ACGME since 1996. Our goal is to provide fellows with an outstanding clinical and research education to become capable independent pediatric gastroenterologists who are ready to pursue careers in academic medicine. We currently have three fellows in our training program with one fellow joining each year.
Weekly Schedule
Monday
| 8:45-9:30 | Inpatient Rounds |
| 9:30-12:00 | Outpatient Clinic & Procedures |
| 13:00-17:00 | Procedures |
Tuesday
| 8:00-8:15 | Peds Radiology Case Discussion |
| 8:45-9:30 | Inpatient Rounds |
| 9:30-12:00 | Outpatient Clinic & Procedures |
| 12:00-13:00 | Peds Surgey - Peds GI Conference |
| 13:00-17:00 | Procedures |
Wednesday
| 8:45-9:30 | Inpatient Rounds |
| 9:30-12:00 | Outpatient Clinic & Procedures |
| 12:00-13:00 | Departmental Pediatric Fellows Core Curriculum Seminar |
| 13:00-17:00 | Outpatient Clinic & Procedures |
Thursday
| 8:00-8:15 | Peds Radiology Case Discussion |
| 8:45-9:30 | Inpatient Rounds |
| 9:30-12:00 | Outpatient Clinic & Procedures |
| 11:00-13:00 | Peds GI Fellows Teaching Seminar |
| 13:00-17:00 | Outpatient Clinic & Procedures |
Friday
| 8:00-9:00 | Pathology - GI Conference |
| 8:45-9:30 | Inpatient Rounds |
| 10:00-12:00 | Outpatient Clinic & Procedures |
| 12:00-13:00 | Grand Rounds |
| 13:00-17:00 | Outpatient Clinic & Procedures |
Bolded sections indicate weekly sub-specialty specific educational sessions.
Education/Conferences
 Pediatric GI Fellows Teaching Seminars
Pediatric GI Fellows Teaching Seminars
These weekly seminars include a variety of teaching sessions on a rotating basis. We discuss core curriculum Pediatric GI topics, and have clinical case conferences, case discussions and journal club presentations. Core curriculum topics are based on the requirements specified by the American Board of Pediatrics. We also have special sessions such as review and interpretation of GI testing including manometry, breath hydrogen testing, capsule endoscopy, and esophageal pH impedance testing. These are practical sessions that allow fellows to see the equipment, learn the technical aspects and evaluate actual patient studies. Clinical case conferences are chosen from patients seen as an outpatient or inpatient services with interesting or difficult diagnosis or a diagnostic and therapeutic dilemma. In Journal Club, we choose the topics to discuss state of the art or cutting edge articles. Case based discussion sessions are run by faculty and aim at assessing the fellows’ knowledge base and thought process in decision making.
Pediatric Fellows Core Curriculum Seminars
Weekly departmental fellow seminars provide opportunities to enhance professional development, explore research options, and advance teaching skills. Our fellows have the opportunity to interact with other pediatric faculty and fellows during these conferences. They have a chance to present their research to the pediatric department, get feedback, and learn how to evaluate their peers' research projects.
 Pediatric Radiology Conference
Pediatric Radiology Conference
We meet with our Pediatric radiologists weekly to discuss recent imaging studies on pediatric GI patients.
Pediatric Surgery Conference
This weekly conference gives the fellows the opportunity to interact with Pediatric Surgery staff and residents. Pediatric GI patients with surgical issues are discussed during these meetings.
Short Bowel/Nutrition Rounds
This involves discussions of inpatients or outpatients with short bowel syndrome or other causes of intestinal failure every month. It includes teaching about pathophysiology, management and discussions with other services including dietary, neonatology, surgery and speech pathology. Guest speakers are frequently invited to present and discuss related topics including GI physiology, nutritional concepts and surgical management.
IBD Rounds
This involves discussions of IBD patients, didactics, protocol development, quality improvement projects, journal club discussions and revision of division's data and outcomes as part of the ImproveCareNow network. It includes family representatives and other services such as dietary, surgery, along with guest speakers from other subspecialties.
Transplant Meeting
These monthly sessions involve meeting with the liver transplant service and discussions of liver failure patients and liver transplant recipients along with didactic sessions.
Pathology Conference
This weekly conference is run by pathologists with extensive experience in GI Pathology. The conference is attended by Pathology staff and residents, Internal Medicine Gastroenterology staff and fellows. Pathology slides are discussed as unknowns. After a pathological diagnosis is reached, patients are briefly presented and a clinicopathological correlation is made. Fellows on clinical service review slides the day before and interpret them with the faculty during these conferences.
We expect our fellows to attend the conferences listed above. A typical weekly work and teaching schedule is outlined here.
Clinical Rotations
 Our inpatient Pediatric GI unit, which is run by pediatric residents, is quite active with over 300 admissions per year. In addition, over 250 consults from various other inpatient services, and over 4000 patient clinic visits are conducted annually. We have an extensive referral base not only within the entire State of Iowa, but also from southern Minnesota, southwestern Wisconsin, western Illinois, eastern Nebraska, and northern Missouri. In addition, fellows participate in some outreach clinics within the State of Iowa.
Our inpatient Pediatric GI unit, which is run by pediatric residents, is quite active with over 300 admissions per year. In addition, over 250 consults from various other inpatient services, and over 4000 patient clinic visits are conducted annually. We have an extensive referral base not only within the entire State of Iowa, but also from southern Minnesota, southwestern Wisconsin, western Illinois, eastern Nebraska, and northern Missouri. In addition, fellows participate in some outreach clinics within the State of Iowa.
As part of the Pediatric Feeding Disorder clinic, our team works with a renowned child psychologist and behavioral feeding specialist, Dr. Linda Cooper-Brown, in managing children with difficult behavioral feeding issues. We also enjoy having an excellent, friendly relationship with our pediatric surgery division.
Fellows perform or are directly involved in a diverse number of procedures. All procedures are supervised by faculty. These include:
- Diagnostic and therapeutic upper endoscopy for foreign body removal, variceal banding, sclerotherapy, stricture dilatation
- Diagnostic and therapeutic colonoscopy for polypectomy, sclerotherapy, stricture dilatation
- Capsule endoscopy placement and interpretation
- Percutaneous endoscopic placement and interpretation
- Endoscopic/fluoroscopic guided gastrojejunal feeding tube placement and replacement
- Percutaneous liver biopsies
- Abdominal paracentesis
- Breath tests
- Intraluminal esophageal impedance and pH probe placement and measurement.
Most procedures are performed in our pediatric GI endoscopy unit. The assistance of a specialized nursing sedation team, supervised by a pediatric anesthesiologist, is available for the majority of our procedures. In high risk or critically ill patients, general anesthesia is available. We perform more than 400 upper endoscopies and more than 150 colonoscopies per year on pediatric patients.
Honors/Recognition
University of Iowa Stead Family Children’s Hospital is the only children’s hospital in Iowa nationally ranked for pediatric care by U.S. News and World Report. Read our June 21, 2023 news release.
- No. 21 in neonatology
- No. 23 in pediatric diabetes and endocrinology
- No. 28 in pediatric orthopedics
- No. 42 in pediatric nephrology
- No. 47 in pediatric neurology and neurosurgery
- No. 48 in pediatric urology
The annual Best Children’s Hospitals rankings recognize the top 50 pediatric facilities across the U.S. in 10 pediatric specialties: cancer, cardiology and heart surgery, diabetes and endocrinology, gastroenterology and gastrointestinal surgery, neonatology, nephrology, neurology and neurosurgery, orthopedics, pulmonology and lung surgery, and urology.
University of Iowa Stead Family Children's Hospital and the Stead Family Department of Pediatrics are recognized nationally for a number of achievements.
Pediatric researchers at the University of Iowa have a long history of breakthrough discoveries in both the clinical and laboratory setting. Meet members of our research team:
Opportunities for Fellows
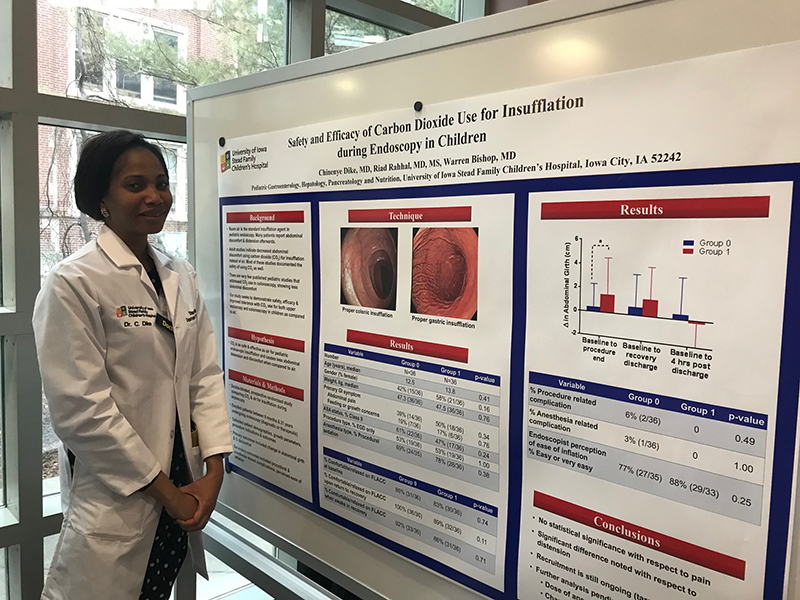
 Our division actively publishes in basic, translational and clinical research realms. All fellows in our program are required to complete two years of research. There are numerous opportunities for basic science lab research in any field of interest across all subspecialties including within our own division. Translational and basic sciences research within our division includes the work of Dr. Aliye Uc, involving mechanisms of pancreatic damage in cystic fibrosis using a porcine model, understanding etiology of acute recurrent and chronic pancreatitis in children (spearheading a multicenter study including 13 other pediatric gastroenterology centers in US and Canada) and the role of heme oxygenase in gut inflammation and oxidative stress. Dr. Warren Bishop and Dr. Riad Rahhal are active in clinical research in the field of constipation, enteral nutritional devices and placement techniques. Fellows also have the opportunity to find research mentors outside the division. Previous fellows have had mentors in Pediatric Critical Care, Neonatology, Immunology, Internal Medicine, Gastroenterology and Hematology Divisions.
Our division actively publishes in basic, translational and clinical research realms. All fellows in our program are required to complete two years of research. There are numerous opportunities for basic science lab research in any field of interest across all subspecialties including within our own division. Translational and basic sciences research within our division includes the work of Dr. Aliye Uc, involving mechanisms of pancreatic damage in cystic fibrosis using a porcine model, understanding etiology of acute recurrent and chronic pancreatitis in children (spearheading a multicenter study including 13 other pediatric gastroenterology centers in US and Canada) and the role of heme oxygenase in gut inflammation and oxidative stress. Dr. Warren Bishop and Dr. Riad Rahhal are active in clinical research in the field of constipation, enteral nutritional devices and placement techniques. Fellows also have the opportunity to find research mentors outside the division. Previous fellows have had mentors in Pediatric Critical Care, Neonatology, Immunology, Internal Medicine, Gastroenterology and Hematology Divisions.
The following is list of some of our division's recent publications:
Al-Zubeidi D, Bishop WP, Rahhal RM. Identifying small bowel intussusception related to a gastroenteric feeding tube. Frontline Gastroenterol. 2:63-64, 2011
Ebach DR, Vanderheyden AD, Ellison JM, Jensen CS. Lymphocytic esophagitis: a possible manifestation of pediatric upper gastrointestinal Crohn's disease. Inflamm Bowel Dis. 17(1):45-9, 2011
Abu-El-Haija M, Stasheff S, Atkins DL, Bishop WP. Rheumatic fever in a patient receiving infliximab therapy for Crohn disease. 52(3):360-1, 2011
Ostedgaard LS, Meyerholz DK, Chen JH, Pezzulo AA, Karp PH, Rokhlina T, Ernst SE, Hanfland RA, Reznikov L, Ludwig PS, Rogan MP, Davis GJ, Dohrn CL, Taft PJ, Rector MV, Hornick E, Nassar P, Samuel M, Richter SS, Uc A, et al. Low Levels of cftr Activity in CFTRDF508/DF508 Pigs Do Not Prevent the Gastrointestinal and Lung Disease of Cystic Fibrosis. Science Translational Medicine 3:74ra24, 2011
Al-Zubeidi D, Rahhal RM. Safety techniques for percutaneous gastrostomy tube placement in Pierre Robin Sequence. JPEN J Parenter Enteral Nutr. 35(3):343-5, 2011
Abu-El-Haija M, Sinkora M, Meyerholz DK, Welsh MJ, McCray PB Jr, Butler J, Uc A. An activated immune and inflammatory response targets the pancreas of newborn pigs with cystic fibrosis. Pancreatology. 11(5):506-15, 2011 Morinville VD, Husain SZ, Bai H, Barth B, Alhosh R, Durie PR, Freedman SD, Himes R, Lowe ME, Pohl J, Werlin S, Wilschanski M, Uc A; on Behalf of the INSPPIRE Group. Definitions of Pediatric Pancreatitis and Survey of Present Clinical Practices. J Pediatr Gastroenterol Nutr. 55(3):261-265, 2012
Abu-El-Haija M, Ramachandran S, Meyerholz DK, Abu-El-Haija M, Griffin M, Giriyappa RL, Stoltz DA, Welsh MJ, McCray PB Jr, Uc A. Pancreatic damage in fetal and newborn cystic fibrosis pigs involves the activation of inflammatory and remodeling pathways. Am J Pathol. 181(2):499-507, 2012
Uc A, Zhu X, Wagner BA, Buettner GR, Berg DJ. Heme oxygenase-1 is protective against nonsteroidal anti-inflammatory drug-induced gastric ulcers. J Pediatr Gastroenterol Nutr. 54(4):471-6, 2012
 Griffin M, Abu-El-Haija M, Abu-El-Haija M, Rokhlina T, Uc A. Simplified and versatile method for isolation of high-quality RNA from pancreas. Biotechniques. 52(5):332-4, 2012
Griffin M, Abu-El-Haija M, Abu-El-Haija M, Rokhlina T, Uc A. Simplified and versatile method for isolation of high-quality RNA from pancreas. Biotechniques. 52(5):332-4, 2012
Al-Zubeidi D, Rahhal RM. Prospective Randomized Comparative Study of Low-Profile Balloon Gastrostomy Tubes in Children. Nutr Clin Pract. 2012 Dec;27(6):812-6
Uc A, Giriyappa R, Meyerholz DK, et al. Pancreatic and biliary secretion are both altered in CF pigs. Am J Physiol Gastrointest Liver Physiol. 2012 Oct;15303(8):G961-8
Malloy L, Jensen M, Bishop W, Divekar A. "Downhill" esophageal varices in congenital heart disease. J Pediatr Gastroenterol Nutr. 2013 Feb;56(2)
Benkov K, Lu Y, Patel A, Rahhal R, Russell G, Teitelbaum J; NASPGHAN Committee on Inflammatory Bowel Disease. Role of thiopurine metabolite testing and thiopurine methyltransferase determination in pediatric IBD. J Pediatr Gastroenterol Nutr. 2013 Mar;56(3):333-40
Al-Zubeidi D, Demir H, Bishop WP, Rahhal RM. Gastrojejunal feeding tube use by gastroenterologists in a pediatric academic center. J Pediatr Gastroenterol Nutr. 2013 May;56(5):523-7
Uc A. Predicting the severity of pediatric acute pancreatitis: are we there yet? J Pediatr Gastroenterol Nutr. 2013 Jun;56(6):584-5
Lerner DG, Li BU, Mamula P, Fishman DS, Kramer R, Goh VL, El-Chammas K, Pentiuk SP, Rothbaum R, Gurrum B, Rahhal RM, Goday PS, Vitola B. Challenges in meeting fellowship procedural guidelines in pediatric therapeutic endoscopy and liver biopsy. JPGN. 2014 Jan;58(1):27-33.
Abu-El-Haiji M, Schultz J, Rahhal R. Effects of 70% ethanol locks on rates of central line infection, thrombosis, breakage and replacement in pediatric intestinal failure. JPGN. 2014 Jun;58(6)
Griffin MA, Restrepo MS, Abu-El-Haija M, Wallen T, Buchanan E, Rokhlina T, Chen YH, McCray PB Jr, Davidson BL, Divekar A, Uc A. A novel gene delivery method transduces porcine pancreatic duct epithelial cells. Gene Ther. 2014 Feb Sui H, Yi Y, Yao J, Liang B, Sun X, Hu S, Uc A, Nelson DJ, Ode KL, Philipson LH, Engelhardt JF, Norris AW. Quantifying insulin sensitivity and entero-insular responsiveness to hyper- and hypoglycemia in ferrets. PLoS One. 2014 Mar 3;9(3):e90519
Morinville VD, Lowe ME, Ahuja M, Barth B, Bellin MD, Davis H, Durie PR, Finley B, Fishman DS, Freedman SD, Gariepy CE, Giefer MJ, Gonska T, Heyman MB, Himes R, Husain S, Kumar S, Ooi CY, Pohl JF, Schwarzenberg SJ, Troendle D, Werlin SL, Wilschanski M, Yen E, Uc A. Design and implementation of INSPIRE(International Study Group of Pediatric Pancreatitis: in search for a Cure). Pediatr Gastroenterol Nutr. 2014 Sep;59(3):360-4
Com G, Uc A. Exercise Intolerance, Malnutrition, Abnormal Sweat Chloride Levels, and Two CFTR Mutations: Is It Cystic Fibrosis? J Pediatr Health Care. 2014 Jul 21
Uc A, Olivier AK, Griffin MA, Meyerholz DK, Yao J, Abu-El-Haija M, Buchanan KM, Vanegas Calderón OG, Abu-El-Haija M, Pezzulo AA, Reznikov LR, Hoegger MJ, Rector MV, Ostedgaard LS, Taft PJ, Gansemer ND, Ludwig PS, Hornick EE, Stoltz DA, Ode KL, Welsh MJ, Engelhardt JF, Norris AW. Glycaemic regulation and insulin secretion are abnormal in cystic fibrosis pigs despite sparing of islet cell mass. Clin Sci (Lond). 2015 Jan;128(2):131-42.
Crockett CD, Bertrand LA, Cooper CS, Rahhal RM, Liu K, Zimmerman MB, Moore SA, Mathews KD. Urologic and gastrointestinal symptoms in the dystroglycanopathies. Neurology. 2015 Feb
Jensen M, Abu-El-Haija M, Bishop W, Rahhal RM. Difficulty Achieving Vitamin D Sufficiency with High Dose Oral Repletion Therapy in Cholestatic Infants. Pediatr Gastroenterol Nutr. 2015 Feb
Schwarzenberg SJ, Bellin M, Husain SZ, Ahuja M, Barth B, Davis H, Durie PR, Fishman DS, Freedman SD, Gariepy CE, Giefer MJ, Gonska T, Heyman MB, Himes R, Kumar S, Morinville VD, Lowe ME, Nuehring NE, Ooi CY, Pohl JF, Troendle D, Werlin SL, Wilschanski M, Yen E, Uc A. Pediatric chronic pancreatitis is associated with genetic risk factors and substantial disease burden. J Pediatr. 2015 Apr;166(4):890-6.
Contact Us
Please direct program-related questions and return applications to one of the following:
Catherine DeGeeter, MD, Pediatric Gastroenterology Fellowship Director
catherine-degeeter@uiowa.edu
Stead Family Department of Pediatrics, Division of Pediatric Gastroenterology
University of Iowa
200 Hawkins Drive, BT 1120-F
Iowa City, IA 52242-1083
319-356-2950 (phone)
319-353-8967 (fax)

Kathy Bell
Pediatric Gastroenterology Fellowship Coordinator
Stead Family Department of Pediatrics - BT 1120-06
University of Iowa Stead Family Children's Hospital
200 Hawkins Drive
Iowa City, IA 52242
Phone: 319-356-2950
Fax: 319-353-8967
Email: kathy-bell@uiowa.edu
