- Fungal, viral, bacterial infections
- Parasitology lecture series
- HIV lecture series
- Tropical Medicine
- Principles of Hospital Epidemiology
- Calls to the Epi Pager
- Infections associated with Transplant
Infectious Disease Fellowship
About the Program
The Infectious Disease Fellowship at University of Iowa Health Care has the following aims:
- To mentor trainees from diverse backgrounds to be outstanding ID clinicians, exemplary in their patient care
- To train leaders of healthcare teams that optimize patient safety and healthcare quality
- To train physician-scholars who expand medical and scientific knowledge through teaching, research, and publication
![]() Program Overview slide presentation
Program Overview slide presentation
Judy Streit, MD, discusses the aims of the program
Dr. Streit discusses where our fellows have gone after completing the program
Ilonka Molano, MD, provides An Associate Program Director’s View
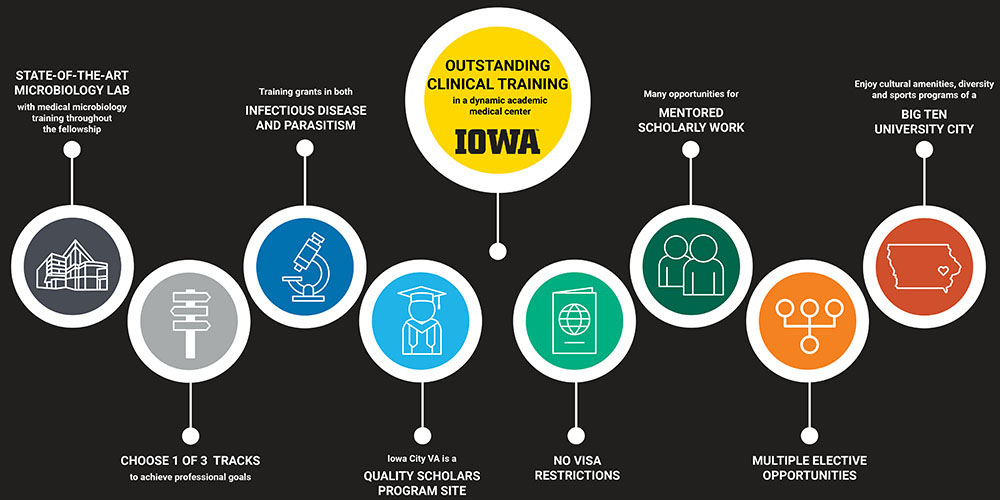
Why Infectious Disease at Iowa?
Sabrina Tan, MD, discusses a newcomer’s experience at the University of Iowa & Iowa City
University of Iowa Health Care as a training center offers the best traditions in academic excellence, collaborative and patient care and innovative research. Outside the hospital, we enjoy Iowa City's vibrant and friendly ambiance, healthy lifestyle, appreciation for the arts and, if you’re so inclined, a boundless enthusiasm for Big Ten sports. Highlights of training at Iowa include:
- Outstanding infectious clinical training in a dynamic quaternary care medical center. We are Iowa’s only academic medical center and a principal benefit of this is a broad referral base. Our trainees will confirm this leads to remarkable diversity of patients and diagnoses. We care for patients from a wide spectrum of socioeconomic backgrounds and from urban or rural environments; patients who are foreign borne or have lived their whole lives in the Midwest. All our patients challenge us to stay committed to life-long learning as clinicians and educators.
- Individualized, customizable fellowship tracks that promote attaining professional goals and advanced experience. About 60% of our graduates work in academic medical centers and 40% in non-academic medical centers.
- Clinical faculty with varied areas of expertise who share a deep commitment to teaching
- Ability to select mentors who will oversee scholarly/research projects
- 100% ID board exam pass rate over more than 10 years
- Busy programs in Transplant ID and HIV care
- Dedicated training in Hospital Epidemiology and Antimicrobial Stewardship
- H-1B and J-1 visa sponsorship
- Opportunities to develop skills as a medical educator
- Opportunities for a research fellowship or other professional development after clinical fellowship
- Community life that is great for families and singles; we enjoy excellent schools, ready access to outdoor adventures and minimal commute times, leaving more time to explore
UI Hospitals & Clinics and the Carver College of Medicine:
- America’s Best Large Employers; #1 in Iowa for healthcare, #6 overall for Iowa; #47 of 500 nationwide for Diversity (Forbes)
- Best Graduate Schools, U.S. News and World Report
- America’s Best Hospitals List, U.S. News and World Report
- America’s Best Children’s Hospitals List, U.S. News and World Report
- Magnet Hospital Designation
- #17 Internal Medicine Residency
Iowa City, a top place to live:
- Iowa City/Coralville, home to the University of Iowa, has a population of approximately 100,000 people, plus 30,000 students
- Nearby Cedar Rapids/Marion has a population of approximately 170,000
- #3 Best Places to Live List, Outside Magazine
- #2 Most Fitness Friendly Places for 2020 (Smartasset); great outdoor activities nearby
- #3 of 10 Best Places to Get a Fresh Start 2019 (Livability)
- #10 of 25 Safest College Campuses
- #13 The 50 Happiest Cities (USA Today)
- World City of Literature, UNESCO; Home of the internationally renowned Iowa Writer’s Workshop
Fellowship Tracks
Fellows select a fellowship track, usually near the end of Year 1. That choice is based on professional aspirations of the fellow and leads to customized training opportunities that provide advanced competence in one/several of a host of areas which position the fellow for success in their desired career paths. All fellows attend IDWeek during Year 2, have IDSA membership sponsored by the Division and complete SHEA’s online fellows’ course in Health Care Epidemiology and Infection Control and Antimicrobial Stewardship, regardless of the track they select.
Clinical/Clinician-Educator Track
In addition to our standard curriculum that prepares fellows to be excellent ID consultants, this track promotes more in-depth clinical experience in specialized niches of ID or through elective rotations outside of ID, such as Allergy-Immunology, Addiction Medicine, or Dermatology. Further, beyond their principal role as a consultant, many ID physicians will lead health care teams in their medical centers, such as antimicrobial stewardship or hospital epidemiology programs. Experiences offered in this track promote acquiring skills in these areas. Specific opportunities include:
- Elective rotations: Allergy/Immunology, Global/Tropical Medicine, Dermatology, Addiction Medicine, NTM Pulmonary Clinic, Pediatric ID, Rheumatology, Ortho ID
- Elective weeks embedded with Antimicrobial Stewardship or Hospital Epidemiology Teams
- Participation in University of Iowa Health Care Quality Leadership Academy
- Participation in Department of Medicine Fellows as Clinician Educators (FACE) Program
- SHEA membership
- Scholarly project such as a QI or Infection Prevention initiative or in medical education
Healthcare Services and Healthcare Quality
This track prepares fellows for infectious diseases careers with special emphasis in hospital epidemiology, health services research or health care quality, including antimicrobial stewardship. It is anticipated that the majority of fellows who select this track are interested in an academic career. Features of this track include the following:
- Availability of IDSA’s Advanced Curriculum for Antimicrobial Stewardship
- Elective time spent embedded with the antimicrobial stewardship team or the program of hospital epidemiology to acquire more advanced experience in these areas
- Attendance at the SHEA Spring meeting
- Nomination to the VA Quality Scholars Program (VAQS) or the VA Health Services Research Fellowship (Note that recently the VA has limited eligibility for visa-holders for these fellowships)
- Paths to a Master’s of Public Health or Master’s of Science in Clinical Investigation if additional years of advanced fellowship are sought, such as through the VAQS program. Coursework in statistics or epidemiology is possible for those not planning on a master’s degree
- Participation in University of Iowa Health Care’s Quality Leadership Academy
- Scholarly work mentored by ID or other University of Iowa faculty who are leaders in Health Services Research, Antimicrobial Stewardship, Hospital Epidemiology or Computational Epidemiology
Physician Investigator Track
This track prepares fellows for careers in ID-related basic science, translational research or clinical investigation.
Physician Investigator Track: to prepare fellows for careers in ID-related bench research or clinical investigation.
- Basic science emphasis
- Membership in specialty society related to research
- Support for 3rd and 4th years of research
- ID Training Grant (T32) (renewal due in 2025)
- Parasitism Training Grant
- Immunology Training Grant
- Mentors/projects available from within the ID Division or from other divisions/departments (e.g., Microbiology, Immunology, Pulmonary Medicine, etc.) Areas of focus within the ID division include:
- Inflammation and innate immunity [see faculty at Inflammation Program]
- Virology (Dr. Jack Stapleton, Dr. Jeff Meier, Dr. Sabrina Tan)
- Parasitology (Dr. Mary Wilson), including collaborative projects with Tropical Medicine Institute in Natal, Brazil (Selma Jeronimo, MD, PhD) and Banaras Hindu University of Varanasi, India
- Vaccine Trials [see Vaccine Education and Research Unit]
- Other labs directed by Carver College of Medicine research faculty or University of Iowa departments
- Department of Microbiology and Immunology
- Scientific meeting during 2nd or 3rd year
- Clinical Investigation
- Mentored involvement in clinical trials (vaccine trials, HIV, neuro-ID, anti-viral therapies) (See Opportunities in Research/Scholarly Project section)
Overview of Clinical Rotations and Other Curriculum Experiences for Year 1 and 2
During the first year the fellow will receive in-depth education in clinical infectious diseases. About 2/3 of required clinical rotations occur in Year 1. Clinical rotations occur primarily at the University of Iowa Health Care University Campus. Some occur at the VA Medical Center (VAMC), which is located across the street from University of Iowa Health Care. Rotations in Transplant ID, Antimicrobial Stewardship and Hospital Epidemiology are part of the curriculum. Fellows have weekly COC clinics (alternating between HIV and general ID). Senior fellows attend several Travel Clinics and Hepatology Clinics when not on service. The fellow will participate in ID Grand Rounds, core curriculum conferences, Journal Club, ID Faculty and Fellows’ conference and departmental fellows’ interdisciplinary conference. Near the end of the first year, each fellow selects a faculty mentor(s) and scholarly project(s). The mentor will guide the fellows’ scholarly work and development during the second year and possibly third and fourth research years.
| Activity | Year 1 | Year 2 | Comment |
|---|---|---|---|
| Team 1 | ∼3 months | ∼1-1.5 months | |
| Team 2 | ∼2.5 months | ∼1.5 months | |
| Team 4 (dedicated) | ∼2 months | ∼1 month | |
| Transplant ID | 1 month | 1 month | |
| Abx Stewardship & Hospital Epi | 1 week each | Per request | |
| COC Clinics | Weekly half-day | Weekly half-day | |
| Micro | 2 weeks | Per request | Plus weekly Micro sessions |
| Scholarly Project/ Research | Selector Mentor and Project | 7-8 months | |
| Travel/Hepatitis Clinic | 4-6 half days each | ||
| Electives | Many available | Derm, Allergy-Immunology, Addiction Medicine, Ortho ID, others |
Team 1
The Team 1 rotation is the principal inpatient general ID consultative service at University of Iowa Health Care. Two and half to three months will be spent on this service in Year 1 and 1.5 months in Year 2. It is the service that challenges our fellows to mature as consultants and teachers, and rewards them with a remarkable learning experience. The fellow manages this team, constituted by the attending, rotating residents, medical students and College of Pharmacy trainees. The service typically sees 120-130 new consults per month. It cares for patients on medicine wards, Medical, Cardiovascular and Surgical Intensive Care Units, Obstetrics-Gynecology and multiple surgical services. All patients are staffed with the attending.
Through rotation on the service, the fellow gains foundational experience in the evaluation and management of patients from highly diverse backgrounds with a broad array of diagnoses. A sampling of our list at any time would reveal patients whose differential diagnoses include endemic fungal, zoonotic or mycobacterial infections. We regularly encounter foreign-borne patients so infections of the tropics are often considered. Patients with iatrogenic immunocompromise or with advanced HIV are cared for by this team.
Fellows also have an opportunity to teach students and residents. Other goals of the rotation include gaining expertise in communicating as a consultant, managing transitions of care, applying principles of antimicrobial stewardship and infection prevention and applying treatment guidelines and current medical literature to individual patients.
Team 2
The Team 2 rotation is the principal outpatient general ID consult service at University of Iowa Health Care. Fellows work 1:1 with the attending to evaluate and manage patients who are new referrals or are seen in follow-up after their hospital discharge. Three to four half-days are spent in clinic per week. Approximately 2.5 months in fellowship Year 1 and 1 to 1.5 months in Year 2 are dedicated to the service. Fellows assigned to this rotation typically also rotate on the inpatient ID service at the VA, which is a low-volume service.
As Iowa’s only comprehensive medical center, we encounter a great breadth of ID diagnoses in the clinic, both common and uncommon. Fellows gain skills in the management of patients receiving complex outpatient antibiotics and how to assess patients during prolonged treatment for illnesses such as tuberculosis, disseminated fungal infection, prosthetic joint infection or infective endocarditis.
As with Team 1, but with a focus on outpatients, fellows gain expertise in communicating as a consultant and apply principles of antimicrobial stewardship, treatment guidelines and current medical literature to individual patients.
Team 4
Team 4 is the ID inpatient rotation that serves the hospitalist teams at University of Iowa Health Care and thus commits its time to consulting on general medicine or occasionally Family Medicine patients. Fellows work 1:1 with the attending in an apprenticeship model which provides time for more discussion about the management of individual patients and feedback to the fellow. About sixty new patients are seen per month on this service. The range of diagnoses and diversity of patients are in keeping with the distinction of being the state’s only comprehensive medical center.
Virology Clinic
Over 700 people living with HIV are cared for at University of Iowa Health Care’s Virology Clinic, which is funded by Ryan White grants. It is a model multidisciplinary clinic that manages the complex medical and psychosocial needs of patients. Fellows gain knowledge of HIV Medicine by managing their own panel of patients (usually 30-40 patients for F2s) whom they follow throughout their fellowship. All patients are staffed 1:1 with an attending. Other members of the care team include case managers/medical social workers, pharmacists, and staff from the Department of Psychiatry. Fellows further strengthen their expertise in HIV Medicine by completing portions of the University of Washington HIV medicine curriculum. A portion of our didactic curriculum is dedicated to HIV Medicine topics to further provide a strong foundation for fellows in this important aspect of ID training.
Transplant Infectious Disease
The Transplant ID Team sees patients who are admitted to the Solid Organ or Hematopoietic Transplant Services. They also consult on patients with acute leukemia or who are CAR-T cell recipients. Lastly, related to their work with the cardiac transplant service, the ID Transplant Team manages patients with LVAD infections. Our medical center has a 24-bed ward that houses HCT or acute leukemia patients. The Solid Organ Transplant program is busy, with 160-180 transplants performed per year, including renal, lung, cardiac and liver transplants. There is an average of 25-30 inpatient consults per month.
Fellows who rotate on the Transplant ID Service staff patients 1:1 with the TP attending. This rotation provides critical experiences so that the fellow is adept in the evaluation and management of highly immunocompromised patients. Fellows come to appreciate the pre-transplant workup and how the post-transplant timeline and features of the immunosuppressive regimen impact the range of infections seen, which in turn informs the differential diagnosis and evaluation. Transplant faculty facilitate a curriculum for the fellows and invite them to participate in multidisciplinary conferences with the surgeons and other medical specialists.
Clinical Microbiology
Our ID fellowship benefits enormously from having an outstanding Clinical Microbiology laboratory on-site. Two to four weeks during Year 1 will be spent in the lab with intensive instruction and hands-on experience with a board-certified clinical microbiologist. Skills gained during the rotation include microscopic examination of specimens, understanding straining and culturing techniques and principles of molecular diagnostics and identification of pathogens. Fellows also learn to interpret susceptibility data and the mechanisms of antimicrobial resistance. In addition to this rotation, Clinical Micro staff also provide tutorials for ID Team 1 and other ID fellows/faculty once or twice per week.
Hospital Epidemiology
The goals of the Year 1 rotation in Hospital Epidemiology are to give the fellows practical and scholarly training in Hospital Epidemiology/Infection Control. During the rotation, fellows will participate in multiple activities of the Program of Hospital Epidemiology at University of Iowa Health Care. The goal is to understand the principles of surveillance and experience a programmatic approach to infection prevention, quality improvement and outbreak investigation. We anticipate this experience will ignite ideas for scholarly work/Quality Improvement. Additional weeks during Year 2 are available upon request.
Fellows complete/attend one of the following: a) SHEA online infection control course (Primer on Healthcare Epidemiology, Infection Control & Antimicrobial Stewardship); or b) SHEA spring or fall meeting in infection prevention.
Antimicrobial Stewardship
Fellows embed in the Antimicrobial Stewardship Teams (AMS) at University of Iowa Health Care and the Iowa City VA for one week during Year 1. Additional time is available upon request. Fellows learn the principles of AMS and how programs at the two facilities promote prudent use of antimicrobials among their providers to optimize patients outcomes and reduce the emergence of resistance. Faculty will facilitate completion of the IDSA AMS Curriculum during the rotation. Faculty provide rotating fellows with several lectures to further strengthen working knowledge of this area.
Travel Clinic
The Travel Clinic at University of Iowa Health Care prepares patients for travel to developing areas during its two half-day clinics per week. Second year fellows spend approximately 4 half days in the Travel Clinic alongside the Travel Clinic staff with the goal that they will adeptly provide patient-specific counseling and recommendation for vaccines or medications before overseas travel to maximize the health and safety of our travelers.
Hepatology Clinic
Patients co-infected with HIV and Hepatitis C have their Hep C treated by Virology Clinic providers. But patients with Hepatitis B or Hepatitis C who are not co-infected with HIV are managed by Hepatology staff. In order for our 2nd year fellows to learn the approach of hepatologists to the management of patients with viral hepatitis, they rotate during several half-day clinics with a Hepatology attending.
Core Curriculum Lecture Series
The ID curriculum includes the consult/clinical assignments, specialty rotations such as Hospital Epi, Antimicrobial Stewardship, Clinical Micro, Travel Clinic and various conferences. For more information about the consult/clinic assignments, specialty rotations or conferences, please see sections dedicated to that information. Another important component of the curriculum is the fellows’ core curriculum lecture series which follows a 2-year cycle. These conferences are given by ID faculty as well as faculty from other divisions and departments, such as GI, Pulmonary, Radiology and Dermatology. The range of topics covered include the following, which is not an exhaustive list:
- Antimicrobial Stewardship
- CNS Infections
- STIs
- Health Equity
- Mimics of ID
- Outbreak Evaluation
- Pneumonia
- Infections associated with biologic agents
- NTM and TB Infections
- Viral hepatitis
- Research Study Design
- Imaging in MSK infections
- CMV/EBV infection
- Tropical Medicine cases
- Derm manifestitions of systemic infections
Conferences
- Infectious Disease Grand Rounds (weekly): Two cases are presented by the fellows or staff as unknowns, discussed with the audience to develop a differential diagnosis, and pertinent literature reviewed
- Core Curriculum Conference (weekly): didactic lectures by faculty cover a broad range of general and specialty ID topics over a 2 year-cycle
- Journal Club (monthly)
- Research conference (weekly): progress on ongoing research activity by members of the Division is presented (ID Faculty and Fellows’ Conference)
- ID Week – Year 2
- University of Iowa Update in Infectious Disease Regional CME Meeting (annually)
- Internal Medicine Grand Rounds and other Departmental conferences
- Clinical Micro tutorials 1-2 times per week
- Departmental Interdisciplinary Fellows’ Curriculum (twice-monthly): presentations on ethics, coding and billing, statistics, sleep deprivation, practice management or other topics that are required for all Internal Medicine fellows [view schedule]
Scholarly Activity during ID Fellowship
Year One
Three months of the first year are not assigned to clinical rotations. These non-scheduled weeks are for study, grand rounds preparation, and to explore with the Career Navigator and Program Leadership what are the fellow’s scholarly interests. Then the fellow meets with possible faculty mentors and develops a project. Under faculty members’ mentorship, we anticipate that by the end of year 1 a project has been selected/proposed.
Scholarly work can include ID-related quality improvement projects, Antimicrobial Stewardship projects or research initiatives, Health Services of Hospital Epi research, Clin Micro projects, clinical reviews/case series, bench research or clinical research. (See Section on Opportunities in Research/Scholarly Projects).
Year Two
Approximately four months of the year are dedicated to clinical rotations. Thus, the second year of fellowship allows for significant time to execute a scholarly project(s). A mentor will guide the project, and a research committee or co-mentor selected from other faculty members will provide additional guidance as needed. Results of the fellows’ work will be presented during the ID Faculty and Fellows’ Conference toward the end of year 2. We encourage fellows to present their work at ID Week or through peer-reviewed publications.
Year Three/Four
A third (and often a fourth) year of advanced fellowship training is available for those who plan a career in academics and are engaged in a fruitful research project during clinical fellowship (see Fellowship Tracks). Building on productive scholarly work initiated during Year 2, the majority of Year 3 and 4 are dedicated to research/scholarly work and possibly course work. (See Advanced Fellowships/Training Section).
Opportunities in Research/Scholarly Projects
Several funding opportunities are listed below for trainees who perform a third (and often a fourth) year of fellowship. There are limitations for several of the grants listed below for fellows’ visas. Tuition support for graduate work has been available for fellows during their research years.
- Infectious Diseases T32 Training Grant (up for renewal in 2025)
- Parasitism Training T32 Grant
- Immunology Training Grant
- VA Quality Scholars Program
- VA Health Services Research Felowship
The Division of Infectious Diseases offers a broad range of research opportunities, with faculty members conducting laboratory research in innate immunity, host-pathogen interactions, parasitology, and virology. There are also opportunities for projects in medical microbiology, antimicrobial stewardship, hospital epidemiology and infection prevention, healthcare delivery and quality improvement, computational epidemiology and with the Vaccine Trials Unit. See below for more detailed information about specific programs or faculty members.
- The Inflammation Program: An interdisciplinary multi-faculty basic science research program that studies innate immunity and host-pathogen interactions with studies related to Staph aureus, Leishmania, and other pathogens. [see the Inflammation Program website]. For faculty names see specific research interests.
- Dr. Stapleton studies the interactions between flaviviruses and immune cells, GB virus C and co-infection and SARS-CoV-2.
- Dr. Winokur leads the University of Iowa Vaccine Trials and Education Unit and the Institute for Clinical and Translational Science (ICTS).
- Dr. Herwaldt is the PI for a CDC Infection Prevention Epi Center grant. Care components include projects in antimicrobial stewardship and infection prevention. She is a PI for a second CDC grant in infection prevention and patient safety.
- Dr. Wilson studies the pathogenesis, biology, immunology, and genetics of Leishmania. She has collaborative projects in Brazil with two adjunct Infectious Diseases faculty members (Drs. Jeronimo and Carvalho) and scholars in India. She coordinates international clinical experiences for trainees.
- Dr. Meier studies basic mechanisms of CMV pathogenesis and latency, and he conducts HIV clinical research.
- Dr. Tan studies polyomovirus infections in immunocompromised hosts; she conducts clinical therapeutic trials and vaccine trials.
- Dr. Polgreen is the cofounder of the interdisciplinary Computational Epidemiology Program at the University of Iowa, which applies bioinformatics to infectious diseases. He is the director of the Emerging Infections Network (EIN), an infectious disease physicians' network for North America, sponsored by the CDC and IDSA, to surveille and gather information on various emerging and re-emerging infections.
- Dr. Ohl is a member of the VA Comprehensive Access & Delivery Research & Evaluation Team (CADRE). He has developed innovative models to provide HIV care to veterans and Hep C care in rural settings via telehealth. He studies healthcare quality and delivery. He directs a program for TelePrEP across the state and is trained in Addiction Medicine.
- Dr. Ince, director of the Transplant Infectious Disease program, also is the physician champion of the UIHC Antimicrobial Stewardship Program (AMS) and is active in the IDSA AMS curriculum and clinical trials for solid organ transplant.
- Dr. Goto is a member of CADRE at the VA. He studies ID-related healthcare outcomes and healthcare quality using VA databases. He is trained in bio-informatics.
- Dr. Livorsi researches healthcare quality and delivery, with a focus on antimicrobial stewardship. He is a member of the VA CADRE group and a Medical Co-Director of the VA AMS team.
- Dr. Sekar specializes in Ortho ID at UIHC and performs MSK infection-related research at the VA and is involved in quality improvement projects.
- Dr. Suzuki conducts research in healthcare delivery and antimicrobial stewardship. He is the Hospital Epidemiologist at the VA.
- Dr. Carvour has an interest in clinical Ortho ID, Ortho ID clinical research and research in health equity for patients with ID diagnoses. She also studies the disparate impact of COVID in the community and the COVID/diabetes syndemic.
- Dr. Prasidthrathsint oversees Clinical Micro projects.
- Dr. Barker is involved in medical education initiatives.
- Dr. Non oversees transplant ID quality improvement projects.
- Dr. Appenheimer and Dr. Kaewpoowat are involved in fellow educational initiatives.
- Dr. Kaewpoowat is involved in a state telehealth program to provide ID care to patients with substance use disorders.
Advanced Fellowships/Training
Training towards several degrees or participation in advanced training programs can occur during a 3rd and 4th year of fellowship. These include:
- Master’s of Public Health degree that is offered through the College of Public Health [more information]
- Master’s of Medical Education Degree (MME). The purpose of this program is develop a community of academic medical faculty with formal training in education who will create and sustain a culture of educational excellence within the College of Medicine, the university, and the medical education community at-large. [more information]
- Masters of Clinical Investigation is a 2-year interdisciplinary program which prepares post-doctoral fellows and junior faculty from the Colleges of Medicine, Nursing, Dentistry, and Pharmacy for careers in clinical research through a structured didactic curriculum in research methods and a mentored research experience.
- Training as a clinical educator can also occur during the 2nd year of clinical fellowship through the Fellows as Clinician-Educators (FACE), a program developed within the Department of Medicine.
- Training in Healthcare Quality and Health Services Research can occur during respective 2-year Iowa City VA programs, after clinical fellowship (VA Quality Scholars or Health Services Research Fellowship). Clinical fellows are nominated per their request.
Select Publications by Infectious Disease Fellows
Arya Zandvakili (graduating 2025)
Zandvakili A, Kobayashi T, Seligman K, Parsons MG, Ford B, Bayon R, Herwaldt LA. A 58-Year-Old Male With a Chronic Sore Throat. Clin Infect Dis. 2023 Sep 11;77(5):792-794. doi: 10.1093/cid/ciad043. PMID: 37696670
Nirmal Muthukumarasamy (graduating 2024)
Muthukumarasamy N, Suzuki H. Epidemiology, Clinical Characteristics, Treatment and Outcome of Mucormycosis during COVID-19 Pandemic in the Veterans Health Administration (VHA) System. IDWeek 2023, Boston. Manuscript in development.
Andrew Simms (graduated 2024)
Simms AJ, Kobayashi T, Schwartzhoff PV, Sekar P. Prosthetic hip infection due to <i>Campylobacter jejuni</i>. BMJ Case Rep. 2022 Mar 10;15(3):e248240. doi:10.1136/bcr-2021-248240. PMID: 35272991; PMCID: PMC8915350.
Michael Olthoff (graduated 2023)
Olthoff M, Kobayashi T, Parsons M, Ford B, Prasidthrathsint K, Non L, Salinas J, Diekema D and Ince D. Impact of metagenomic next-generation sequencing on clinical decision-making at an academic medical center, a retrospective study, Iowa, 2020–2022. Antimicrobial Stewardship and Healthcare Epidemiology, 2024; 4, e39, 1-4.
Joseph Tholany (graduated 2022)
Tholany, J, Kobayashi, T, Marra, AR, Schweizer, ML, Samuelson, RJ, Suzuki, H. Impact of infectious diseases consultation on the outcome of patients with enteroccoal bacteremia: a systemic literature review and meta-analysis. OFJD, ofac200, epublished April 12, 2022; https://doi.org/10.1093/ofid/ofac200
Matthew Smith (graduated 2022)
Smith M, Kobayashi T, Sekar P. Antibody testing to distinguish between histoplasmosis and blastomycosis. BMJ Case Rep. 2021 May 31;14(5):e243587. doi: 10.1136/bcr-2021-243587.
Livorsi, DJ, Nair, R, Dysangco, A, Aylward, A, Alexander, B, Smith, MW, Kouba, S, Perencevich, EN. Using audit-and-feedback to improve antimicrobial-prescribing in Emergency Departments: a multicenter quasi-experimental study in the Veterans Health Administration. Open Forum Infectious Diseases, ofab186, April 14, 2021.
Smith, M. W., Carrel, M., & Goto, M. (2023). County-level spatiotemporal distribution of fluoroquinolone-resistant Enterobacteriaceae in outpatient settings of the Veterans’ Health Administration, 2000–2017. Infection Control & Hospital Epidemiology, 44(9), 1497-1499
Carrel, M., Shi, Q., Clore, G. S., Hasegawa, S., Smith, M., Perencevich, E. N., & Goto, M. (2024). Assessing the potential for improved predictive capacity of antimicrobial resistance in outpatient Staphylococcus aureus isolates using seasonal and spatial antibiograms. Antimicrobial Resistance & Infection Control, 13(1), 1-6.
Smith, M. & Herwaldt, L (2023). Nasal decolonization: What antimicrobials and antiseptics are most effective before surgery and in the ICU. American Journal of Infection Control. 51(11), A64-A71.
Smith, M., Crnich, C., Donskey, C., Evans, C. T., Evans, M., Goto, M., ... & Perencevich, E. N. (2024). Research agenda for transmission prevention within the Veterans Health Administration, 2024–2028. Infection Control & Hospital Epidemiology, 1-10.
Smith, M. W., O’Shea, A. M., & Wray, C. M. (2023). Health Care and Climate Change—Telemedicine’s Role in Environmental Stewardship. JAMA network open, 6(1), e2253794-e2253794
Smith, M. W., Hernandez, L. V., Lee, P., Martinello, R. A., Singh, H., & Sherman, J. D. (2024). Single-Use vs. Reusable Duodenoscopes: How Infection Knowledge Gaps Are Driving Environmental Harm and What Can Be Done. Gastroenterology, S0016-5085
Fernando Casado Castillo (graduated 2021)
Casado-Castillo F, Kobayashi T, Sekar P, Streit J, Molano De Pena I. Prosthetic hip infection due to Salmonella enterica serovar Enteritidis. IDCases. 2021 May 23;25:e01170. doi: 10.1016/j.idcr.2021.e01170.
Kobayashi T, Trannel A, Holley SA, Alsuhaibani M, Abosi OJ, Jenn KE, Meacham H, Sheeler LL, Etienne W, Dains A, Casado F, Kukla ME, Ward E, Ford B, Edmond MB, Wellington M, Diekema DJ, Salinas JL. COVID-19 Serial Testing among Hospitalized Patients in a Midwest Tertiary Medical Center, July-September 2020. Clin Infect Dis. 2020 Oct 26:ciaa1630. doi: 10.1093/cid/ciaa1630. Online ahead of print.PMID: 33103196
Edin Pujagic (graduated 2021)
Kobayashi, T, Bogdanic, F, Pujagic, E, Goto, M. Isolated Splenic Abscess due to Salmonella Berta in a Healthy Adult. BMJ Case Rep. 2020 Apr 7;13(4). pii: e235318. doi: 10.1136/bcr-2020-235318
Htay Phyu (graduated 2020)
Phyu, H, Edmond, MB, Kobayashi, T. Metronidazole-Induced Encephalopathy ID Cases. 2019 Sep 7; 18:e00639 doi: 10.1016/j.idcr.2019.e00639. eCollection 2019. PMID 31692663
Phyu, H, Kobayashi, T., Rastogi, P, Cho, C. Vancomycin-induced linear Immunogloblulin A bullous dermatosis. BMJ Case Reports, Dec 2019, 12(12) e233281: DOI: 10.1136/bcr-2019-233281 PMID 31822537
Phyu H, Kobayashi T, Ford, B, Molano, I. Splenic abscess as a rare presentation of blastomycosis. BMJ Case Rep. 2020 Feb 13; 13(2). Pii: e234062. Doi: 10.1136/bcr-2019-234062 PMID 32060116
Takaaki Kobayashi (graduated 2020)
Kobayashi T, Trannel A, Holley SA, Alsuhaibani M, Abosi OJ, Jenn KE, Meacham H, Sheeler LL, Etienne W, Dains A, Casado F, Kukla ME, Ward E, Ford B, Edmond MB, Wellington M, Diekema DJ, Salinas JL. COVID-19 Serial Testing among Hospitalized Patients in a Midwest Tertiary Medical Center, July-September 2020. Clin Infect Dis. 2020 Oct 26:ciaa1630. doi: 10.1093/cid/ciaa1630. Online ahead of print.PMID: 33103196
Kobayashi T, Amram AL, Gehrs K, Diekema D, Barker J. A 52-Year-Old Man With Uveitis and Altered Mental Status. Clin Infect Dis. 2021 Mar 1;72(5):873-875. doi: 10.1093/cid/ciaa051.PMID: 33667312
Kobayashi T, Salinas JL, Ten Eyck P, Chen B, Ando T, Inagaki K, Alsuhaibani M, Auwaerter PG, Molano I, Diekema DJ. Palliative care consultation in patients with Staphylococcus aureus bacteremia. Palliat Med. 2021 Apr;35(4):785-792. doi: 10.1177/0269216321999574. Epub 2021 Mar 24.PMID: 33757367
Kobayashi T, Marra AR, Schweizer ML, Ten Eyck P, Wu C, Alzunitan M, Salinas JL, Siegel M, Farmakiotis D, Auwaerter PG, Healy HS, Diekema DJ. Impact of Infectious Disease Consultation in Patients With Candidemia: A Retrospective Study, Systematic Literature Review, and Meta-analysis. Open Forum Infect Dis. 2020 Aug 3;7(9):ofaa270. doi: 10.1093/ofid/ofaa270. eCollection 2020 Sep.PMID: 32904995
Kobayashi T, Beck B, Miller A, Polgreen P, O'Shea AMJ, Ohl ME. Positive Predictive Values of 2 Algorithms for Identifying Patients with Intravenous Drug Use-Associated Endocarditis Using Administrative Data. Open Forum Infect Dis. 2020 Jun 1;7(6):ofaa201. doi: 10.1093/ofid/ofaa201. eCollection 2020 Jun.PMID: 32607386
Kobayashi T, Jenn KE, Bowdler N, Malloy R, Holley S, Izakovic T, Kukla ME, Abosi O, Dains A, Meacham H, Diekema DJ, Edmond MB, Salinas JL. Reduction in abdominal hysterectomy surgical site infection rates after the addition of anaerobic antimicrobial prophylaxis. Infect Control Hosp Epidemiol. 2020 Dec;41(12):1469-1471. doi: 10.1017/ice.2020.386. Epub 2020 Aug 28.PMID: 32856576
Kobayashi T, Meacham H, Alsuhaibani M, Holley S, Marra AR, Edmond MB, Diekema DJ, Hartley PG, Salinas JL. Occupational tuberculosis exposures and conversion rates can guide deimplementation of annual tuberculosis skin test screening. Infect Control Hosp Epidemiol. 2021 Jan;42(1):123-124. doi: 10.1017/ice.2020.205. Epub 2020 Jun 2.PMID: 32484119
Kobayashi T, Clore GS, Kukla ME, Alzunitan M, Kritzman J, Abosi O, Puig-Asensio M, Marra AR, Diekema DJ, Edmond MB, Salinas JL. Insertion site inflammation was associated with central-line-associated bloodstream infections at a tertiary-care center, 2015-2018. Infect Control Hosp Epidemiol. 2021 Mar;42(3):348-350. doi: 10.1017/ice.2020.445. Epub 2020 Oct 9.PMID: 33032671
Kobayashi T, Ford B, Fujita N, Appenheimer AB. Ocular Actinomycosis Mimicking Meningioma. Open Forum Infect Dis. 2020 May 19;7(6):ofaa170. doi: 10.1093/ofid/ofaa170. eCollection 2020 Jun.PMID: 32529000
Kobayashi T, Lawler E, Samra H, Ford B, Sekar P. Prosthetic Finger Joint Infection Due to Aspergillus terreus. Open Forum Infect Dis. 2020 Dec 13;8(1):ofaa614. doi: 10.1093/ofid/ofaa614. eCollection 2021 Jan.PMID: 33511236
Kobayashi T, Ando T, Streit J, Sekar P. Current Evidence on Oral Antibiotics for Infective Endocarditis: A Narrative Review. Cardiol Ther. 2019 Dec;8(2):167-177. doi: 10.1007/s40119-019-00148-4. Epub 2019 Sep 18.PMID: 31535282
Sammantha Kouba (graduated 2020)
Kouba SJ, Kobayashi T, Blount RJ, Herwaldt L. Atrial flutter as a rare manifestation of leptospirosis. BMJ Case Rep. 2020 Aug 26:13(8)e237693 PMID 32847893
Kouba S, Kobayashi T, Meier J, Sekar, P. Osseous blastomycosis mimicking malignancy. BMJ Case Rep. 2020 Aug 25;13(8):e237688 PMID 32843470
Livorsi, DJ, Nair, R, Dysangco, A, Aylward, A, Alexander, B, Smith, MW, Kouba, S, Perencevich, EN. Using audit-and-feedback to improve antimicrobial-prescribing in Emergency Departments: a multicenter quasi-experimental study in the Veterans Health Administration. Open Forum
Hiroyuki Suzuki (graduated 2019)
Suzuki H, Perencevich EN, Livorsi DJ, Alexander B, Beck BF, Richardson KK, Goto M. Attributable mortality due to fluoroquinolone and extended-spectrum cephalosporin resistance in hospital-onset Escherichia coli and Klebsiella spp bacteremia: A matched cohort study in 129 Veterans Health Administration medical centers. Infect Control Hosp Epidemiol. 2019 Aug;40(8):928-931.
Suzuki H, Perencevich EN, Alexander B, Beck BF, Goto M, Lund BC, Nair R, and Livorsi DJ. Inpatient Fluoroquinolone Stewardship Improves the Quantity and Quality of Fluoroquinolone-prescribing at Hospital Discharge: A Retrospective Analysis among 122 Veterans Health Administration Hospitals. Clin Infect Dis. 2020 Aug 22;71(5):1232-1239.
Suzuki H, Perencevich EN, Nair R, Livorsi DJ, Goto M. Excess Length of Acute Inpatient Stay Attributable to Acquisition of Hospital-Onset Gram-Negative Bloodstream Infection with and without Antibiotic Resistance: A Multistate Model Analysis. Antibiotics 2020, 9(2), 96
Suzuki H, Clore G, Perencevich EN, Hockett-Sherlock S, Goto M, Nair R, Branch-Elliman W, Richardson K, Gupta K, Beck BF, Alexander B, Balkenende E, Schweizer ML. Development of a Fully Automated Surgical Site Infection Detection Algorithm for Use in Cardiac and Orthopedic Surgery Research. Infect Control Hosp Epidemiol. 2021 Feb 23;1-6.
Suzuki H, Perencevich EN, Goto M, Nair R, Puig-Asensio M, Ernst E, Livorsi DJ. A Comprehensive Assessment of Carbapenem Use across 90 Veterans Health Administration Hospitals with Defined Stewardship Strategies for Carbapenems. J Antimicrob Chemother. 2021 Feb 1;dkab008.
Interdisciplinary Fellowship Conference
Below is an example of the Department of Internal Medicine Common Curriculum Schedule. It is shared between Fellows from all divisions of the Department.
Fellows as Clinician Educators (FACE)
The Fellows as Clinician Educators (FACE) Program is designed to introduce future clinician-educators to a set of skills which may be of use in their career. The program presents concepts of educational design and research, lecture development, evaluation, observation and feedback. At the conclusion of the program, FACE participants are required to develop a teaching portfolio.
How to Apply
| Thank you for your interest in infectious diseases, an incredibly rich, diverse, and rewarding specialty. As is evidenced by the ongoing COVID-19 pandemic, the bounds of our specialty know no limits, spanning pathogenesis, clinical care, disaster planning, infection control and prevention, immunology and vaccine development, public health, social determinants of health, diagnostic testing, and communication skills. While the task is daunting, we will overcome this pandemic, in large part thanks to the tireless efforts of infectious diseases experts and advocates everywhere.
IDSA, the ID Training Program Directors’ Committee, and all ID program directors understand that the fellowship application season falls during this complex and chaotic time. We also understand that some anticipated ID clinical elective rotations may not be undertaken, that anticipated research projects may not be completed, and that previously envisioned letters of recommendation may not materialize. We assure you that we will review all applications mindful of these realities, and we will not hold schedule changes imposed by COVID-19 against any applicant. We strongly encourage anyone who is considering applying for ID fellowship training to apply, and not to withhold your application because of these concerns. We welcome your interest in infectious diseases and our program, and we look forward to meeting many of you on the interview trail this year, whether in person or remotely |
Applications are only accepted through the Electronic Residency Application System (ERAS).
US residents should contact their Dean's Office or ERAS at https://students-residents.aamc.org/training-residency-fellowship/applying-fellowships-eras/.
International residents should contact the ECFMG at http://www.ecfmg.org/eras/index.html. Sponsorship of J-1 visas is preferred (on occasion H-1b).
An ECFMG certificate must accompany the ERAS application.
A background of research experience is not essential. However, we would encourage applicants who have a strong interest in pursuing an academic Infectious Diseases career. Our research programs range from Clinical Infectious Diseases (antibiotic stewardship, transplantation), Epidemiology (infection control, emerging infections network), Translational Research (vaccines, clinical trials, antibiotic/antifungal resistance), and Basic Research (virology, parasitology, bacteriology, and innate and adaptive immunity).
A complete ERAS application includes:
- Curriculum vitae
- Statement of the applicant's long-term career goal and field of interest
- Dean's letter
- Three letters of support
- Copies of ECFMG scores for Steps I, II, and III (if completed)
- Notarized copies of applicant's transcripts for USMLE Steps 1, 2, and 3
- Medical school transcript
- An unmounted recent photograph of applicant must accompany application or be provided at time of interview.
All applicants must also register with the National Resident Matching Program (Phone: 202-828-0566).
The NRMP numbers for our program is 1203146F0.
The deadline for applications is September 30.
Selected candidates will be invited to interview.
Application Deadline
The deadline for applications is September 30.
Board Certification
Medical specialty certification in the United States is a voluntary process which serves multiple purposes for the trainee and the public.
Certification is
- one mission of the training program to produce trainees who meet board eligibility criteria;
- distinguishes a physician as someone with a distinct level of expertise;
- provides more opportunities when applying for employment;
- presents resources and tools by the ABMS;
- a commitment to life-long improvement for providing the best patient care; and
- elevates physicians into the ranks of doctors committed to the highest standards of healthcare.
For more information visit the American Board of Internal Medicine for specifics on board certification requirements.
Eligibility Criteria
Qualifications for candidates include (1) an MD degree (or equivalent), (2) completion or expected completion of three years of residency training in Internal Medicine, with Board Eligibility or Certification by the American Board of Internal Medicine, by the initiation of Infectious Diseases Fellowship training
Interview Information
At the interview, perspective candidates will receive an overview of the program and tour of the facilities. They will also meet individually with key faculty members that may include any or all of the following: the program director, other Infectious Diseases faculty, and the department chair.
Our People
Program Leadership

Judy A. Streit, MD
Director, Infectious Diseases Fellowship Program
Clinical Professor of Internal Medicine
Email: judy-streit@uiowa.edu

A. Benjamin Appenheimer, MD
Associate Director, Infectious Diseases Fellowship Program
Clinical Associate Professor of Internal Medicine
email: alpheus-appenheimer@uiowa.edu

Ilonka Molano, MD
Associate Director, Infectious Diseases Fellowship Program
Clinical Associate Professor of Internal Medicine
email: ilonka-molano@uiowa.edu
Current Faculty
The Department of Internal Medicine has a faculty of nearly 300 professionals whose clinical, teaching, and research expertise spans the entire discipline of medicine.
Infectious Diseases Division Faculty
Department Faculty (alphabetical listing)
Other Faculty with Infectious Diseases interest
Perencevich, Eli N., MD, MS (General Internal Medicine)
Ford, Bradley, MD, PhD (Pathology)
Current Fellows

Alexandria Burtness-Guard, DO (F1)
Medical School: Des Moines University College of Osteopathic Medicine
Residency: University of Iowa Des Moines Internal Medicine

Renate Gyenge, DO (F2)
Medical School: Ohio University Heritage College of Osteopathic Medicine
Residency: NE Ohio Medical University

Shinya Hasegawa, MD (F2)
Medical School: Tokyo Medical and Dental University
Residency: Western Michigan University
Yacoub Sallam, MD (F1)
Medical School: University of Jordan Faculty of Medicine
Residency: Cleveland Clinic

Sebastian Sanchez Lopez, MD (F1)
Medical School: Universidad de Antioquia Facultad de Medicina Colombia
Residency: Texas Tech

Arya Zandvakili, MD, PhD (F2)
Medical School: University of Cincinnati
Residency: University of Iowa
Research Groups
Host Defense Group
| Botond Bánfi, MD, PhD Associate Professor of Anatomy and Cell Biology |
Polly Ferguson, MD Professor of Pediatrics |
Prajwal Gurung, PhD Associate Professor of Medicine (Infectious Diseases) |
| John T. Harty, PhD* Professor of Microbiology |
Priya Issuree, PhD Assistant Professor of Medicine (Infectious Diseases) |
Julia Klesney-Tait, MD, PhD Professor of Medicine (Pulmonary) |
| Kevin Legge, PhD Professor of Pathology |
Thorsten Maretzky, PhD Assistant Professor of Medicine (Infectious Diseases) |
Paul McCray, MD Professor of Pediatrics |
| Craig Morita, MD, PhD Professor of Medicine (Rheumatology) |
William M. Nauseef, MD* Emeritus Professor of Medicine (Infectious Diseases) |
Elizabeth Newell, MD Associate Professor of Pediatrics |
| Stanley Perlman, MD, PhD* Professor of Microbology |
Mary E. Wilson, MD Professor of Medicine and Microbiology |
Molecular Pathogenesis Group
Viral Pathogenesis Subgroup
| Zuhair Ballas, MD Professor of Medicine (Allergy) |
Gail Bishop, PhD Professor of Medicine and Microbiology |
Charles Grose, MD Professor of Pediatrics |
| Hillel Haim, PhD Research Assistant Professor of Microbiology |
Aloysius J. Klingelhutz, PhD Professor of Microbiology |
Wendy Maury, PhD Professor of Microbiology |
| Jeffery Meier, MD Professor of Medicine (Infectious Diseases) |
Stanley Perlman, MD, PhD Professor of Microbiology |
David Price, PhD Professor, Department of Biochemistry |
| Richard J. Roller, PhD Professor of Microbiology |
Jack Stapleton, MD Professor of Medicine (Infectious Diseases) |
C. Martin Stoltzfus, PhD Professor of Medicine (Microbiology) |
| Joseph Zabner, MD Professor of Medicine (Pulmonary) |
Bacterial Pathogenesis Subgroup
| John T. Harty, PhD Professor of Medicine (Microbiology) |
Li Wu, PhD Professor and Chair, Department of Microbiology |
Paul McCray, MD* Professor of Pediatrics |
| Craig Morita, MD, PhD* Professor of Medicine (Rheumatology) |
William M. Nauseef, MD* Emeritus Professor of Medicine (Infectious Diseases) |
Patricia L. Winokur, MD Professor of Medicine (Infectious Diseases) |
Associate Members |
||
| Steven Clegg, PhD Professor of Medicine (Microbiology) |
Daniel J. Diekema, MD, MS Emeritus Professor Medicine (Infectious Diseases) |
Timothy L. Yahr, PhD Emeritus Professor of Microbiology |
| Bradley Jones, PhD Professor of Microbiology |
Eukaryotic Pathogenesis Subgroup
| Noah Butler, PhD Professor of Microbiology and Immunology |
John T. Harty, PhD Professor of Microbiology |
Louis V. Kirchhoff, MD, MPH Professor of Medicine (Infectious Diseases) |
| W. Scott Moye-Rowley, PhD Professor of Physiology & Biophysics |
Mary E. Wilson, MD Professor of Medicine (Infectious Diseases) |
Hospital epidemiology/Healthcare Research
| Karen Brust, MD, Clinical Associate Professor of Medicine (Infectious Diseases) | Michihiko Goto, MD, MSCI, FACP Associate Professor of Medicine (Infectious Diseases) |
Loreen Herwaldt, MD Professor of Medicine (Infectious Disease) |
| Takaaki Kobayashi, MD, MPH Adjunct Assistant Professor of Medicine (Infectious Diseases) | Daniel Livorsi, MD, MSC Associate Professor of Medicine (Infectious Diseases) |
Michael Ohl, MD, MPH Professor of Medicine (Infectious Disease) |
| Eli Perencevich, MD, MS Professor of Medicine and Epidemiology |
Philip Polgreen, MD, MPH Professor of Medicine (Infectious Disease) |
Clinical and Vaccine Research (ID Division)
| Patricia Winokur, MD Professor of Medicine (Infectious Disesse) |
Jack Stapleton, MD Professor of Medicine (Infectious Disease) |
Jeffery Meier, MD Professor of Medicine (Infectious Disease) |
Clinical Microbiology Research
| Bradley Ford, MD, PhD Clinical Assistant Professor of Pathology |
J. Stacey Klutts, MD, PhD Clinical Associate Professor of Pathology |
Kunatum (Jin) Prasidthrathsint, MD Clinical Associate Professor of Medicine (Infectious Diseases) |
Chair, Department of Internal Medicine

Upinder Singh, MD
Chair and DEO, Department of Internal Medicine
Professor of Medicine–Infectious Diseases