Allergy/Immunology Fellowship
About the Program
The Division of Immunology at the University of Iowa offers a 2 year ACGME accredited fellowship program in Allergy/Immunology. The program is designed to provide the trainee with in depth knowledge and experience in the diagnosis and treatment of allergic, immunologic and complex disorders in both pediatric and adult patients. In addition, trainees have the opportunity to learn about and participate in clinical, translational and/or basic research in the field of allergy and immunology. The Program Evaluation Committee, with input from the fellows, reviews the educational program on a regular basis to assure that all ACGME and ABAI requirements are met and to address areas for improvement and strategies to optimize program quality.
Al lergy/Immunology Fellowship Program Highlights
lergy/Immunology Fellowship Program Highlights
- Adult and pediatric patient care experiences in a broad array of allergic and immunologic disorders
- Experience in a multidisciplinary Drug Allergy Clinic
- Clinical and research opportunities in food allergy
- Exposure to state-of-the-art equipment and facilities in the new Children’s Hospital (Opened in 2017)
- Experience in a complex disorders clinic and inpatient program
- Participation in Iowa’s Severe Combined Immunodeficiency (SCID) Newborn Screening Program
- Participation in the annual Quality Improvement and Patient Safety Symposium and the Current Topics in Allergy & Clinical Immunology Conference
- Research opportunities in the Center of Immunology and Immune-Based Disorders
- Exposure to the Journal of Allergy and Clinical Immunology
- Fellows as Clinician Educators (FACE) Program
- Masters in Medical Education Program, reserved for fellows interested in an academic career as clinical educators
Program Mission
Our fellowship program has been accredited by the ACGME since 1981 and has trained more than 30 fellows who have gone on to successful careers in private practice or academic medicine. The mission of our fellowship program is to empower learners to take advantage of the unique breadth of opportunities offered through the University of Iowa to advance careers in teaching, scholarship, and patient care in academic and/or community settings.
Our goals for the training program include:
- Assuring that training occurs in a supportive environment that embraces a culture of physician well-being and resilience;
- Engaging in outreach to the medical and lay community to promote allergy/immunology awareness and health;
- Collaborating with providers throughout the institution to further systems-based approaches to improve health care delivery to our allergy/immunology patients.
General Duties of Fellows
The Allergy/Immunology fellowship program in the Division of Immunology at the University of Iowa represents a two-year commitment for physicians who have completed training in Internal Medicine, Pediatrics or combined Medicine-Pediatrics and who wish to pursue subspecialty training in the field. The program is structured to meet all of the 24-month requirements set forth by both the ACGME and the American Board of Allergy and Immunology (ABAI). In addition, there is an option for additional years of training in research for those individuals with prior research experience who are interested in pursuing a career in academic medicine. Year 1 of the fellowship emphasizes clinical training in the adult and pediatric outpatient clinics, as well as an inpatient consultative experience. Year 2 of the fellowship provides some additional time for more involvement in a scholarly project, leadership and teaching experiences, and increased responsibilities to assure transition to competence in the independent care and management of children and adults with common as well as rare allergic and immunologic disorders. Educational conferences, board review sessions, journal clubs, interesting cases sessions, hands-on workshops and research conferences are held throughout the entire 24-month program and serve as the framework for core curriculum and team-based learning necessary to acquire the skills to practice independently and competently in the field of allergy/immunology.
The Division of Immunology houses fellowship programs in both Allergy/Immunology and Adult Rheumatology. We now have an approved pathway for physicians interested in pursuing dual certification in Allergy/Immunology and Rheumatology. The dual pathway requires acceptance into each of the individual fellowships, as well as final approval by the ABAI and the ABIM Rheumatology Subspecialty Board. The pathway enables the fellow to complete requirements for board eligibility in both subspecialties in three years as opposed to the traditional four years.
Year One
Fellows ordinarily begin their two-year training program in July. Year One emphasizes clinical training and includes approximately four 1/2-day outpatient clinics (including pediatric and adult Continuity of Care Clinics [COC]), rotations on allergy/immunology inpatient consults and complex disorders inpatient consults. The fellow also gains experience in various procedural skills including allergy skin testing, allergen immunotherapy, pulmonary function testing, food challenges, drug challenges and desensitization, patch testing and the use of immunoglobulin and other immunomodulatory drugs. First year fellows begin their year with direct faculty supervision for the first three months. For example, a faculty member and the fellow respond to consults together in order to train the fellow in identifying the important points in history, physical exam, evaluation/diagnostic testing and therapeutic planning. The fellow assumes increasing responsibilities throughout the two year period but will always be supervised by a faculty member before signing off on any patient. During the first year it is anticipated that the fellow will also attend one national meeting and participate in the Division's annual CME course.
 Throughout Year One, the fellow is expected to attend and participate in Immunology Grand Rounds, journal clubs and all teaching conferences, as well as attend other selected research seminars and Divisional meetings. Training and certification in Human Subjects Research and Bioethics, as well as Animal Care and Use (if appropriate) is also completed at the beginning of year one.
Throughout Year One, the fellow is expected to attend and participate in Immunology Grand Rounds, journal clubs and all teaching conferences, as well as attend other selected research seminars and Divisional meetings. Training and certification in Human Subjects Research and Bioethics, as well as Animal Care and Use (if appropriate) is also completed at the beginning of year one.
During the first three months of training the fellow is expected to meet with each faculty member to discuss research interests and scholarly activities. By the end of October, the fellow will meet with the Training Program Director to discuss the projects he/she is interested in pursuing and a research project and mentor will be selected. The fellow and identified mentor is expected to meet on a regular basis. In addition, the fellow will meet at least twice a year with their scholarly oversight committee which includes the research mentor, Program Director, and the Division Director. The first year fellow will be asked to present a research in progress talk towards the end of the academic year. The scholarly project can include bench, clinical, or translational research, clinical trials or chart review. Selecting a specific research project does not preclude the fellow from collaborating with other faculty members on individual case reports, phase III drug trials, etc. The fellows are urged to develop their own protocols with the supervision of the faculty, and all scholarly projects should be hypothesis driven.
Year Two
 Year Two provides the opportunity for trainees to complete their required clinical experiences in adult and pediatric allergy/immunology and also assures completion of all procedural skill requirements. Fellows also complete required clinical rotations in Pediatric Rheumatology and Adult HIV, as well as an educational rotation in the Immunopathology laboratory. The fellow spends three-four ½ days per week in the outpatient clinics, including their COC clinic. The second year fellow also assumes a leadership role on the inpatient consultation team, assumes increasing responsibilities for patient care and teaching of first year fellows, residents and medical students. Time is provided for ongoing scholarly work and the fellow will continue to meet on a regular basis with both their research mentor as well as their Scholarly Oversight Committee. It is expected that the fellow will submit at least one abstract to a national meeting (either the American College of Allergy, Asthma and Immunology [ACAAI], the American Academy of Allergy, Asthma and Immunology [AAAAI], or the Clinical Immunology Society (CIS). It is hoped that the fellow will have at least one manuscript accepted for publication in a peer reviewed journal.
Year Two provides the opportunity for trainees to complete their required clinical experiences in adult and pediatric allergy/immunology and also assures completion of all procedural skill requirements. Fellows also complete required clinical rotations in Pediatric Rheumatology and Adult HIV, as well as an educational rotation in the Immunopathology laboratory. The fellow spends three-four ½ days per week in the outpatient clinics, including their COC clinic. The second year fellow also assumes a leadership role on the inpatient consultation team, assumes increasing responsibilities for patient care and teaching of first year fellows, residents and medical students. Time is provided for ongoing scholarly work and the fellow will continue to meet on a regular basis with both their research mentor as well as their Scholarly Oversight Committee. It is expected that the fellow will submit at least one abstract to a national meeting (either the American College of Allergy, Asthma and Immunology [ACAAI], the American Academy of Allergy, Asthma and Immunology [AAAAI], or the Clinical Immunology Society (CIS). It is hoped that the fellow will have at least one manuscript accepted for publication in a peer reviewed journal.
Throughout Year Two, the fellow is expected to attend and participate in Immunology Grand Rounds, journal clubs, board review sessions, research conferences, hands-on workshops and case-based conferences. The second year fellow will be asked to assist with planning of these various educational activities as well as the Division CME course. He/She will serve a leadership and teaching role in these various activities. In addition the fellow is provided the opportunity to attend one additional educational meeting during the second year (i.e. Clinical Immunology Society [CIS] Summer School, Aspen Allergy Conference, ACAAI/AAAAI Board Review Course, ATS Annual Meeting).
Opportunities for Additional Training
The Division of Immunology has options for an additional 1-2 years of training for those individuals with prior research experience desiring an intensive research experience in preparation for a future career in academic medicine as a physician-scientist. Fellows wishing to pursue this pathway should identify such interest to their research mentor, the Program Director and the Division Director by the spring of their first year of fellowship. The trainee will be asked to work with their research mentor to apply for and successfully receive funding for this research pathway either through the competitive application process for an NIH T32 training grant or equivalent. For fellows planning an academic career as a clinician-educator, the Division has options for trainees to participate in the “Fellows as Clinician Educator” course during Year Two. In addition, fellows wishing to pursue a Master’s in Medical Education should discuss this option with the Program Director and the Division Director by the spring of their first year of fellowship.
Call and Consult Experience
 Fellows rotate responsibility for day-time consults and after hours calls/consults throughout the two year program. The call/consult experience involves the evaluation and management of both adult and pediatric inpatients. The fellow is the first contact person for all consults and patient calls after hours. Evening and weekend call is taken from home. If there is a consult, the fellow will see the patient first and then contact the assigned faculty member. The faculty member will then come in to the Hospital and see the patient with the fellow. Please note that work hours are not to exceed 80 hours per week averaged over four weeks and fellows have at least one full day out of seven away from program duties, averaged over a month's time.
Fellows rotate responsibility for day-time consults and after hours calls/consults throughout the two year program. The call/consult experience involves the evaluation and management of both adult and pediatric inpatients. The fellow is the first contact person for all consults and patient calls after hours. Evening and weekend call is taken from home. If there is a consult, the fellow will see the patient first and then contact the assigned faculty member. The faculty member will then come in to the Hospital and see the patient with the fellow. Please note that work hours are not to exceed 80 hours per week averaged over four weeks and fellows have at least one full day out of seven away from program duties, averaged over a month's time.
Conference and Teaching Program
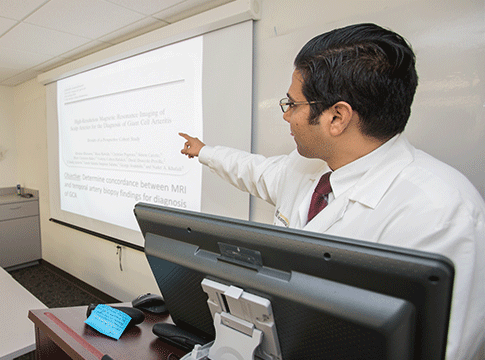 Immunology Grand Rounds are held on Wednesdays at 1:00 p.m. Presentations are given on a wide range of clinical and research topics in the field of clinical immunology. Fellows are required to present at least one Grand Rounds talk each year. Journal clubs are held approximately once a month and fellows are required to present at least one journal club a year. Other educational activities on Wednesday afternoons include interesting cases, hands-on workshops and core curriculum didactic lectures. Sessions rotate week by week. Fellows are required to attend the Internal Medicine Fellowship Lecture series on Thursdays at 1:00 p.m. and are encouraged to regularly attend either Internal Medicine or Pediatric Grand Rounds. A required Allergy/Immunology Board Review session is held weekly. Finally, fellows have the opportunity to attend the Immunology Group Seminars sponsored by the Immunology Graduate Program.
Immunology Grand Rounds are held on Wednesdays at 1:00 p.m. Presentations are given on a wide range of clinical and research topics in the field of clinical immunology. Fellows are required to present at least one Grand Rounds talk each year. Journal clubs are held approximately once a month and fellows are required to present at least one journal club a year. Other educational activities on Wednesday afternoons include interesting cases, hands-on workshops and core curriculum didactic lectures. Sessions rotate week by week. Fellows are required to attend the Internal Medicine Fellowship Lecture series on Thursdays at 1:00 p.m. and are encouraged to regularly attend either Internal Medicine or Pediatric Grand Rounds. A required Allergy/Immunology Board Review session is held weekly. Finally, fellows have the opportunity to attend the Immunology Group Seminars sponsored by the Immunology Graduate Program.
Supervision and Duty Hours
All fellows in the Division of Immunology at University of Iowa Hospitals & Clinics are supervised by faculty. Fellows are assigned to clinics that are staffed by a faculty member dedicated to that clinic. In addition, fellows have their own Pediatric and Adult Continuity of Care (COC) Clinics that are staffed by a faculty member. Fellows are given increasing responsibility for patient care as they progress through the training program, however, every UI Hospitals & Clinics patient seen by a fellow is also seen by a faculty physician in the Division. In the Allergy Clinic at the Iowa City VA Health Care System, all patients seen by a first year fellow must also be seen by the faculty member staffing that clinic. Patients seen by an upper level fellow in the VA Clinic are discussed with the faculty member staffing that clinic and in some instances will also be seen by the faculty member depending on the nature of the clinical problem.
All inpatient consultations during regular working hours are first seen by the fellow and then staffed by faculty members. Weekend and on-call consultations are first seen by the fellow and then staffed within 24 hours by the faculty on-call. A faculty member is always available for fellow supervision.
Policy on Duty Hours
The Division of Immunology policy regarding fellow work hours follows the guidelines set by UI Hospitals & Clinics and by ACGME. This policy applies to all Allergy-Immunology fellows. Work hours are not to exceed 80 hours per week and fellows have at least 1 full day out of 7 away from program responsibilities, averaged over a month’s time. Fellows do not take in house call. Evening and weekend call responsibilities are rotated among the fellows.
Fellows are actively involved in preparing the on call schedule, which is reviewed by the Program Director. Conflicts with this call schedule are directed to the Program Director for resolution. Note that the on-call fellow covers the University of Iowa Hospitals & Clinics adult and pediatric areas as well as the Iowa City VA Hospital.
Fellows are required to submit their duty hours on MedHub on a weekly basis, and this is monitored by the Program, the Department, and the GME office.
Competencies and Evaluation
Throughout the year, fellows are evaluated by supervising faculty. Competency based assessment tools include simulated chart reviews, conference presentation/teaching evaluations, procedural skills evaluation, in-training examinations, patient surveys, and 360° Evaluations. Fellows are required to evaluate the faculty and the training program on a semi-annual basis. Fellows are required to maintain an accurate and up-to-date ACGME on-line case and procedure log. Fellows are required to maintain an accurate and up-to-date learning portfolio documenting accomplishments towards achieving competency in the areas of patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism and system-based practice.
Fellows meet with the Program Director on a semi-annual basis to review progress and receive feedback. The Clinical Competency Committee assists with completion of the ACGME Allergy/Immunology Milestone assessments.
Major Areas of Research
- Tumor immunology
- Immunology of alcoholism
- Immunologic and clinical changes in immunotherapy
- In vitro correlates of atopic diseases
- Immune tolerance
- Transplantation research
- Natural killer cells
- Biological response modifiers
- Mechanisms of graft vs. host disease
- Primary immunodeficiency
- Mechanisms of allergic inflammation
- Food allergy
- Drug allergy evaluation and desensitization
Interdisciplinary Fellowship Conference
Below is an example of the Department of Internal Medicine Common Curriculum Schedule. It is shared between Fellows from all divisions of the Department.
Fellows as Clinician Educators (FACE)
The Fellows as Clinician Educators (FACE) Program is designed to introduce future clinician-educators to a set of skills which may be of use in their career. The program presents concepts of educational design and research, lecture development, evaluation, observation and feedback. At the conclusion of the program, FACE participants are required to develop a teaching portfolio.
Allergy/Immunology & Adult Rheumatology Dual Certification Pathway
For interested, highly qualified candidates, the Division offers a pathway that enables achievement of board eligibility in rheumatology and allergy/immunology in three years. Applicants interested in this pathway should review all information for both fellowships on our web site, and then submit their ERAS application to the rheumatology program, with an indication of interest and focused career goals related to the dual certification pathway in their personal statement.
How to Apply
All interviews will be virtual in 2023 due to the COVID-19 pandemic
Applications are only accepted through the Electronic Residency Application System (ERAS).
Fellows can apply beginning July 1, and the programs can upload the applications beginning July 15.
US residents should contact their Dean's Office or ERAS at https://students-residents.aamc.org/training-residency-fellowship/applying-fellowships-eras/.
International residents should contact the ECFMG at http://www.ecfmg.org/eras/index.html
An ECFMG certificate must accompany the ERAS application.
A complete ERAS application includes:
- curriculum vitae
- statement of the applicant's long-term career goal and field of interest
- dean's letter
- three letters of support from individuals who can assess the applicant's potential for a career in allergy-immunology from firsthand knowledge of the applicant's performance
- copies of ECFMG scores for Steps I, II, and III (if completed)
- Certified copies of applicant's transcripts for USMLE Steps 1, 2, and 3
- medical school transcript
- Recent digital photograph (.jpg) of applicant must accompany application or be provided at time of interview
- All applicants must also register with the National Resident Matching Program (Phone: 202-828-0566).
The NRMP number for our program is 1203020F0.
If you have any questions, contact Patty Bruffey-Thoene.
Application Deadline
Applications and all supporting documents must be submitted through ERAS. We review all completed applications submitted through September 1, however, once we have filled our interview slots we do not review further applications. Interviews typically occur in August and September.
Board Certification
Medical specialty certification in the United States is a voluntary process which serves multiple purposes for the trainee and the public.
Certification is
- one mission of the training program to produce trainees who meet board eligibility criteria;
- distinguishes a physician as someone with a distinct level of expertise;
- provides more opportunities when applying for employment;
- presents resources and tools by the ABMS;
- a commitment to life-long improvement for providing the best patient care; and
- elevates physicians into the ranks of doctors committed to the highest standards of healthcare.
For more information visit the following sites for specifics on board certification requirements.
Eligibility Criteria
Qualified applicants to the University of Iowa Allergy/Immunology Fellowship Program are those who have successfully completed medical school and a medicine residency program at an accredited institution.
Interview Information
At the interview, perspective candidates will receive an overview of the program and tour of the facilities. In addition to meeting with the program director and key faculty members, applicants have an opportunity to meet with our current fellows and other members of our medical team (allied health providers, nurses, pharmacists) and administrative team (program coordinator, support staff).
Our People
Program Leadership

Amy M. Dowden, MD
Allergy/Immunology Fellowship Program Director
Clinical Professor of Internal Medicine and Pediatrics

Diana Bayer, DO
Allergy/Immunology Fellowship Associate Program Director
Clinical Professor of Pediatrics and Internal Medicine

Benjamin Davis, MD, PhD
Interim Director, Division of Immunology
Clinical Associate Professor of Internal Medicine and Pediatrics
Contact Us

Patty Bruffey Thoene
Allergy/Immunology Fellowship Coordinator
Department of Internal Medicine - C42-B GH
The University of Iowa Carver College of Medicine
200 Hawkins Drive
Iowa City, IA; 52242-1009
Email: patricia-bruffeythoene@uiowa.edu

Denise Floerchinger
Internal Medicine Fellowship Program Administrator
Phone: 319.356.2732
Email: denise-floerchinger@uiowa.edu
Current Faculty
The Department of Internal Medicine has a faculty of nearly 300 professionals whose clinical, teaching, and research expertise spans the entire discipline of medicine.
Zuhair Ballas, MD
Professor of Internal Medicine - Immunology

Diana Bayer, DO
Clinical Associate Professor of Pediatric Allergy-Immunology
Secondary Appointment(s): Internal Medicine
Lauren Bobst, PA-C
Physician Assistant - Allergy and Immunology
Benjamin Davis, MD, PhD
Clinical Associate Professor of Internal Medicine - Immunology
Secondary Appointment(s): Pediatrics

Amy Dowden, MD
Clinical Professor of Internal Medicine - Immunology
Secondary Appointment(s): Pediatrics
Mary Beth Fasano, MD, MSPH
Professor Emeritus of Internal Medicine - Immunology
Secondary Appointment(s): Pediatrics
Brooke Harrison, ARNP
Advanced Registered Nurse Practitioner - Immunology
Carolyn Kay-Buckelew, ARNP
Advanced Registered Nurse Practitioner - Allergy and Immunology
Bharat Kumar, MD, MME
Clinical Assistant Professor of Internal Medicine - Immunology

Deanna McDanel, PharmD, BCPS, BCACP
Clinical Pharmacy Specialist - Allergy and Immunology
Department of Pharmacy
Secondary Appointment(s): Internal Medicine
Immunology Division Faculty (Allergy/Immunology and Rheumatology)
Department Faculty (alphabetical listing)
Current Fellows
Allergy/Immunology Fellowship Pathway
Truman Nguyen, MD (F1)
Medical School: University of Wisconsin
Residency: University of Iowa

Mackenzie Hines, MD (F2)
Medical School: University of Iowa
Residency: University of Iowa
Allergy/Immunology and Rheumatology Dual Certification Pathway

Amir Abidov, MD (F2)
Medical School: University of Arizona
Residency: Lankenau Medical Center
Chair, Department of Internal Medicine

Upinder Singh, MD
Chair and DEO, Department of Internal Medicine
Professor of Medicine–Infectious Diseases