General Surgery Residency
Your surgical residency at Iowa is designed for career success.
At Iowa, you’ll be well prepared, whether you follow a path toward general surgery or continue for a fellowship in a surgical subspecialty. We take pride in offering our residents a superior education aimed at providing leading-edge patient care and advancing our field through basic-science and clinical research. Train where you will care for the broadest set of cases, to build your expertise from the most common to the most complex surgical conditions.
Grow Here
Our programs attract residents who are prepared to maximize their clinical and research training in a high-energy and supportive learning environment.
About the Program
Surgery excels in its three-part mission to be a leader in teaching, research, and patient care.
You’ll benefit from exposure to renowned faculty members who are committed to your growth and development.
We have a strong reputation nationally, built on the excellence for our training programs.
Our residents are prepared for success along whatever career path they choose—academics, subspecialties, or private practice.
A comprehensive learning environment
Residency training is a top priority for all members of the surgery faculty.
More than half of our residents enter fellowship programs. The close work you’ll do alongside fellows in our programs will afford you many opportunities to determine your career pathway.
You’ll move through a well-engineered program that provides you with increasing responsibility from year one to year five.
You’ll learn in an environment that encourages scholarly pursuits. We provide you with opportunities to conduct original clinical and basic science research.
We invite you to explore how livable Iowa City is for balancing work demands with a great healthy lifestyle. Iowa City offers unmatched cultural and recreation opportunities right outside the hospital’s doors.
History
The College of Medicine was established in the late 1860s by Dr. Washington Freeman Peck, who initiated the efforts to create a state-supported medical school in Iowa City. The College of Medicine’s first class began in 1870, where Dr. Peck served as the first Dean of the Faculty and Chairman of the Department of Surgery, in which he served for 20 years.
After Dr. Peck served as the first chairman, the department has had such notable chairs as Dr. Frank Peterson, Dr. Sidney Ziffren, Dr. Carol Scott-Conner, and now Dr. Ronald Weigel, who were or are all leaders in their surgical specialties and dedicated to surgical education. An example of this dedication to surgical education was highlighted through the development of the Ziffren Professorship, which was established to honor Dr. Sidney Ziffren and is designated to be held by the Director of the Surgical Residency Training Program. The current holder of the Ziffren Professorship is Dr. John Sharp, who has completed both a general surgery residency and vascular fellowship here at the University of Iowa Hospitals and Clinics.
The residency training program itself has evolved and grown through many decades, facing numerous changes in both society and in the medical community; however, the program has and will continue to provide a superior education developed through a resident-centered atmosphere.
Rotation Schedule

| FIRST YEAR | SECOND YEAR | ||
|---|---|---|---|
| Specialty | # of Blocks | Specialty | # of Blocks |
| Emergency General Surgery | 1-2 | Pediatric Surgery | 2 |
| GI Surgery | 1-2 | Surgical Intensive Care Unit | 2 |
| Pediatric Surgery | 1-2 | Vascular Surgery | 2 |
| Surgical Oncology | 1-2 | VA General Surgery | 2 |
| Transplant Surgery | 1-2 | Cedar Rapids | 1-2 |
| VA General Surgery | 1-2 | Emergency General Surgery | 1-2 |
| Vascular Surgery | 1-2 | Burns | 1 |
| Cardiothoracic Surgery | 1 | Night Float | 1 |
| Cedar Rapids | 1 | ||
| Night Float | 1 | ||
| THIRD YEAR | FOURTH YEAR | ||
| Specialty | # of Blocks | Specialty | # of Blocks |
| Breast Surgery | 2 | Cardiothoracic Surgery | 2-3 |
| Plastic Surgery | 2 | Trauma | 2-3 |
| Mason City | 2 | GI Surgery | 2 |
| Transplant Surgery | 2 | Pediatric Surgery | 2 |
| Vascular Surgery | 2 | Vascular Surgery | 2 |
| Emergency General Surgery | 1-2 | Night Float | 1-2 |
| GI Surgery | 1-2 | Chief Rotation | 1 |
| Night Float | 1 | ||
| FIFTH YEAR | |||
| Specialty | # of Blocks | ||
| Surgical Oncology | 2-3 | ||
| Emergency General Surgery | 2 | ||
| GI Surgery | 2 | ||
| VA General Surgery | 2 | ||
| Vascular Surgery | 2 | ||
| Chief Rotation | 1 | ||
| Night Float | 1 |
Rotation Descriptions
Breast Surgery
Residents learn procedures related to the surgical treatment of breast conditions, such as cyst aspiration, FNA, and percutaneous core needle biopsy.
Burns
As the only Burn Treatment Center in Iowa, this service provides exposure to a diverse set of patients of all ages and with all mechanisms of burn and soft tissue injury. In addition to treating patients with chemical, electrical, and thermal energy burns, residents will care for individuals with severe frostbite injuries and necrotizing soft tissue infections. Residents learn management of the acutely injured burn patient, wound care, and skin harvesting and grafting.

Cardiothoracic Surgery
Residents rotating with this service are involved with cardiac surgeries on pediatric and adult patients. Working with thoracic surgeons, they receive training in procedures including esophagectomies, resections of mediastinal masses, and thoracoscopic and open lung resections. They will also gain experience in heart and lung transplantation.
Cedar Rapids
Second year residents have the opportunity to rotate at the Cedar Rapids based Mercy General Surgery Clinic, comprised of University of Iowa Department of Surgery faculty members. While on this rotation, residents are involved in acute care, general, and trauma cases that include appendectomies, breast biopsies, colon and rectal surgery, gallbladder surgery, general laparoscopic surgery, and vascular access surgery.
Chief Rotation
This month is an opportunity for senior residents to gain experience in surgical cases of their interest as well as to work with endoscopists to further their upper and lower endoscopy skills. Residents in their "chief month" meet regularly with the department chair to review the weekly operative cases and they also lend assistance by covering cases for the surgical teams as needed.

Emergency General Surgery
This is the general surgery consult service for the University. Residents rotating on this service develop the skills to efficiently and thoroughly evaluate patients and treat for "bread and butter" issues including appendicitis, cholecystitis, bowel obstruction, hernia, and perforated viscera.
GI Surgery
This service encompasses the breadth of benign and malignant diseases of the small bowel, colon, rectum and anus. Residents rotating on this service learn lower endoscopy and are trained in open, laparoscopic, and robotic approaches to a variety of colorectal conditions. Additionally, this service encompasses the University of Iowa Obesity Surgery, a bariatric Center of Excellence, where residents gain significant experience in gastric bypass surgery, laparoscopic experience performing ventral and inguinal herniorrhaphy, paraesophageal hernia repair and Nissen fundoplication, cholecystectomies via a minimally-invasive approach.
Mason City
Third year residents have the opportunity to rotate at a private practice hospital, Mercy Medical Center in Mason City, Iowa. The majority of the resident's time is spent operating and cases range from outpatient hernia and laparoscopic cholecystectomies to mastectomies, colon resections, and any general surgery emergencies that present. Residents also take trauma call and are responsible for evaluating and stabilizing patients. Housing is provided.
Night Float
This team is a combination of Trauma and Emergency General Surgery services. Residents are responsible not only for evaluation and treatment of trauma patients and general surgery consults, but they also provide cross-coverage for surgical patients admitted during the day.
Pediatric Surgery
Residents rotating on this service are exposed to elective and emergent surgeries for all ages, from premature neonates to teenagers. The team also manages pediatric trauma patients. It works closely with the Pediatric Gastroenterology team as well as the NICU and PICU. Across all pediatric ages, residents gain varied experience operating in the neck, thorax, and abdomen through both open and laparoscopic approaches. Common neonatal procedures performed include closure of gastroschisis and omphalocele, treatment of tracheoesophageal fistulas, repair of congenital diaphragmatic hernias, and management of necrotizing enterocolitis.
Plastic Surgery
Residents learn a diverse set of procedures such as scar revision, liposuction, post-mastectomy breast reconstruction, component separation for hernia repair, and microvascular free flaps.
Surgical Intensive Care Unit
Rotating in the SICU provides an unparalleled opportunity to care for a diverse set of critically ill patients. Working with critical care specialists trained in surgery, anesthesia, medicine, and pharmacy, residents are part of a multidisciplinary team managing patients with complex needs. Residents learn ventilator management, vascular access, tracheostomy and PEG placement, and neurologic monitoring.
Surgical Oncology
Residents learn to diagnose, stage, and determine optimal treatment for a variety of malignancies including melanoma, sarcomas, gastric cancer, pancreatic cancer, and neuroendocrine tumors. Multidisciplinary tumor board conferences facilitate integration of information from a number of specialties to determine the optimal care plan for patients. Additionally, this team encompasses surgical treatment of thyroid and parathyroid conditions.
Transplant
This service specializes in liver, pancreas, and kidney transplants, as well as in hepatobiliary procedures. Residents are trained in the harvesting of organs for transplant, including laparoscopic donor nephrectomies, as well as in the transplantation of these organs. Hepatobiliary procedures performed include those for benign and malignant conditions. Perioperative management of the transplant and hepatobiliary patient is emphasized. Residents will work closely with members of the Transplant Hepatology and Transplant Nephrology teams.
Trauma
UIHC the only Level 1 Trauma Center in the state, caring for seriously injured patients. Residents on the Trauma service learn to rapidly assess and treat these patients, as well as to manage their overall cares once stabilized. The trauma team works closely with other surgical sub-specialties to coordinate and meet patients' treatment needs. All general surgery residents will be ATLS certified. Common procedures performed on this service include: FAST exam, chest tube placement, central line placement, tracheostomies, and trauma laparotomies.
Vascular Surgery
Residents rotating on this service will receive training in procedures including: open and endovascular repair of aneurysms, carotid endarterectomy, creation of arterial venous fistulas for hemodialysis, and lower extremity vascular bypass. The mid-level resident is in charge of the outpatient endovascular procedures performed in the cardiac cath lab which include primarily diagnostic and therapeutic angio/venograms as well as vascular access.

Veterans Affairs Hospital - General Surgery
This is the general surgery consult service for the Iowa City Veterans Affairs hospital, located across the street from the University of Iowa. Similar to the University service, residents develop the skills to efficiently and thoroughly evaluate patients and treat for "bread and butter" issues including appendicitis, cholecystitis, bowel obstruction, hernia, and perforated viscera. Additionally, renal transplants and thoracic procedures are performed at this VA.
Veterans Affairs Hospital - Vascular Surgery
Residents rotating on this service will receive training in procedures including: open and endovascular repair of aneurysms, carotid endarterectomy, creation of arterial venous fistulas for hemodialysis, and lower extremity vascular bypass.
Conference Schedule
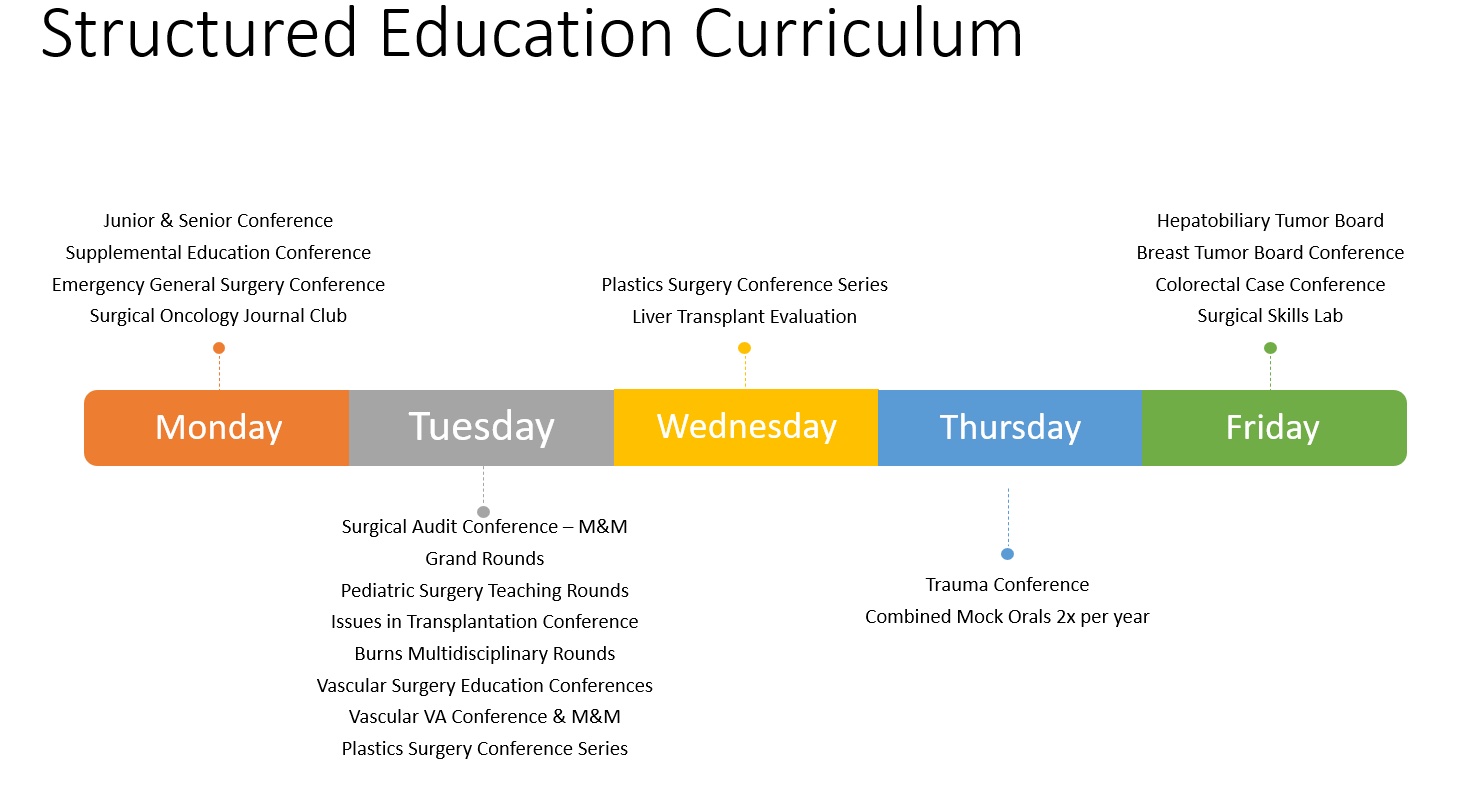
This is a sample weekly conference schedule. Those marked with an asterisk are mandatory for all general surgery residents. The others are service-specific and are attended by residents and the faculty on their respective services.
| Monday | ||
|---|---|---|
| 7 a.m. | Junior Resident Education Conference* | |
| 7 a.m. | Senior Resident Education Conference* | |
| 7:30 a.m. | Kidney Transplant Evaluation Conference | |
| 8 a.m. | Supplemental Education Conference* | |
| Noon | Emergency General Surgery Conference | |
| 5 p.m. | Surgical Journal Club Conference | |
| Tuesday | ||
| 6:30 a.m. | Surgical Audit Conference- M&M* | |
| 7 a.m. | Thoracic Tumor Board | |
| 7 a.m. | Plastics Surgery Conference Series | |
| 7:15 a.m. | Grand Rounds* | |
| 8 a.m. | Issues in Transplantation Conference | |
| 8 a.m. | Vascular VA Conference & M&M | |
| 8:30 a.m. | Burns Multidisciplinary Rounds | |
| 11 a.m. | Pediatric Surgery Teaching Rounds | |
| 4 p.m. | Vascular Surgery Education Conferences | |
| Wednesday | ||
| 3 p.m. | Liver Transplantation Evaluation Conference | |
| 4:30 p.m. | Plastics Surgery Conference Series | |
| Thursday | ||
| 7 a.m. | Trauma Conference | |
| Friday | ||
| 7 a.m. | Hepatobiliary Conference | |
| 12:30 p.m. | Colorectal Case Conference | |
| 1 p.m. | Breast Tumor Board Conference | |
| 1 p.m. | Surgical Skills Lab* |
Conference Descriptions
Junior Conference
This conference is held on Mondays at 7 a.m. and is for the PGY1s, PGY2s, and PGY3s. The format of this conference utilizes a flipped classroom educational approach, where residents will be assigned weekly modules from SCORE (the General Surgery Resident Curriculum Portal). At the start of the conference residents will complete a short quiz, which will be reviewed by assigned faculty who serve as content experts and who will bring interactive case scenarios to be discussed after the review of the quiz.
Senior Conference
This conference is held on Mondays at 7 a.m. and is for the PGY4s and PGY5s. The format of this conference focuses on scheduled topics where faculty experts moderate sessions that are much like the real oral boards. Brief feedback is provided immediately and formal feedback is provided every 6 months.
Supplemental Education Conference
This conference is held on Monday morning from 8 a.m. to 9 a.m. for all residents. The focus of this conference shifts throughout the year to address additional education topics separate from or building on the SCORE curriculum. From July 1 – Sept 1 we hold “Summer School” covering a variety of clinical topics such as: Patient Handoffs, Consults, Presenting Patients, Discharge Planning, Medical Student Teaching, as well as Giving and Receiving Feedback. From September – January the focus shifts to ABSITE review sessions. February through June, we focus on comprehensive topics, such as; Wellness, Quality Improvement, and Narrative Medicine.
ABSITE Review Conference
General surgery residents take the American Board of Surgery In-Training Exam (ABSITE) every year. The residency program is dedicated to helping residents succeed on this exam, and thus every year beginning in August a weekly ABSITE Review Conference is held. This conference is facilitated by one of our junior faculty members and focuses on one ABSITE topic a week.
Surgical Audit
This conference is held on Tuesdays at 6:30 a.m. The content of this conference focuses on cases selected to present and an appropriate literature review in order to improve patient care and reduce complications. Residents selected to present cases, work with faculty members in the development of presentation.
Grand Rounds
This conference is held Tuesdays from September through June on Tuesdays at 7:15 a.m. As surgical science and practice progresses rapidly, a need exists to continuously keep abreast of advances in surgical education, practice, and research. Utilizing visiting experts and local faculty members, development in these areas are formally presented and discussed.
Skills Lab
Skills lab sessions are held monthly and as needed. A skills lab curriculum is developed allowing for the residents, based upon level, to learn skills in a controlled environment allowing for verifiable proficiency to be achieved. Sessions are led by department faculty and include formal presentations followed by hands-on practice.
Surgical Skills Lab
The UI Hospitals & Clinics Center for Procedural Skills and Simulation provides skills training to all residents in the University of Iowa General Surgery Residency Program. The Resident Skills Training Curriculum is administered through the Skills Center with the goal of providing learner-focused surgical skills education in a low stress environment that facilitates more complex learning in the patient environment. The skills curriculum includes weekly skills modules with didactic sessions and hands-on training facilitated by an expert faculty member. The curriculum utilizes computerized simulation, simulated models, and animal parts for the training modules. Highlighting the skills training are multiple live animal labs annually involving residents of different levels performing multiple basic and complex laparoscopic and open procedures.
Within the curriculum, several surgical skills are now being taught to proficiency in the Verification of Proficiency program. This program involves not only the usual education module, but adds a pre-test, scripted regimen of routine practice, and a post-test to determine technical competency with standardized criteria for proficiency.
In addition to the skills curriculum, the Fundamental of Laparoscopic Surgery Curriculum is administered within the Skills Center usually during the PGY3 year. Other planned events throughout the year include the Skills Boot Camp, cadaver labs, and a vascular anastomosis competition.
Staff

John Keech, MD
Director of Procedural Skills, Center for Procedural Skills and Simulation

Julie Hartman
Instructional Services Manager
Johnson Ding
Procedural Skills and Simulation Center Coordinator
Research Opportunities

Different from many residency programs, ours will immerse you in research that’s informed by your own curiosity and passion. You’ll not only have the support of a faculty mentor, but the laboratory and computing resources of a major academic medical center.
Our residents have used their research experiences as a foundation for a career of pursuing the great questions of modern medicine. They regularly present their findings at conferences and publish in scholarly journals.
Our physician researchers ask the kinds of questions that help move laboratory discoveries to innovative new treatments in the clinical setting.
Learn more about our department’s research.
The importance of research
Research is an important part of the daily activities of all academic surgeons. The continuing commitment to productive scholarship, embodied by research, as much as a commitment to communicative scholarship, exemplified by teaching, distinguishes the academic surgeon from his/her colleague in nonacademic practice.
The obvious benefit of research to our patients and to the community is improved care. Less obvious but equally important benefits are the atmosphere of open and rigorous inquiry, the constant questioning, and the intellectual stimulation the research programs provide to their participants—faculty, residents, and medical students.
There are numerous opportunities to become involved in basic science and/or clinical research. Those interested in basic science can work in the laboratories of surgical faculty ranging from those in the Transplant, Gastrointestinal Surgery, Minimally-invasive, and Bariatric Surgery divisions to those in the Surgical Oncology and Endocrine divisions. Residents interested in basic science can spend two years in the lab devoted to research, which leads to the development of many projects that are presented at regional and national meetings. Additionally, many of our faculty members perform clinical research and welcome resident participation. Please use the following link for information concerning research within the Department of Surgery.
Our facilities
Our laboratory complex includes animal operating rooms and laboratories, completely staffed and equipped to carry out nine animal procedures simultaneously. Our specialty laboratories include peripheral vascular, gastric motility, analytical chemistry, transplant, neurosurgery, tissue culture, surgical bacteriology, kidney preservation, and shock units. In a typical year, more than 1,000 experimental procedures are performed in the laboratories. The facilities permit study of such experimental procedures as heart valve replacement in large animals and bile duct cannulation studies in guinea pigs and heterotopic heart transplantation in mice and rats. There is also active research in surgical oncology, studying the sequence of mutations and the localization of predisposition genes for cancers.
Finally, the general surgery residency training program allows three of our residents after their PGY2 year to step out for two years. These two years are flexible and can be dedicated to two years of research; a combination of a fellowship and research; completing a graduate degree such as an MBA or a Masters in Medical Education or other practical options. After completing these two years, the resident transitions back into the program at the PGY3 level.
Research Presentations
Residents completing basic science and/or clinical research have successfully submitted abstracts to present at local, regional, and national meetings. Both platform and poster presentations have been given at meetings hosted by the Academic Surgical Congress, American Burn Association, American Colleges of Surgeons, American Society of Colon and Rectal Surgeons, Society of Surgical Oncology, and many others.
A listing of selected titles of presentations given over the 2017-2018 academic year is as follows:
- Outcomes for Gastrostomy Placement in the Setting of Pediatric Peritoneal Dialysis
- Biologic Effects and Long-Term Outcomes in Neonatal Gastroschisis (BELONG) Study
- Nipple-Sparing Mastectomy with Immediate Reconstruction: A Safe and Effective Option for Overweight and Obese Women?
- MnT4MPyP Enhances Ascorbate-Induced Radiosensitization in Pancreatic Cancer (PDAC)
- Ascorbate Decreases Circulating Tumor Cells (CTCs) in Mice
- Treatment & Prognosis of Rectal Squamous Cell Carcinoma: Analysis of the National Cancer Database
- Invasive Fungal Infections in Burns
- A population-based Validation of the New AJCC Subclassification of Anal Squamous Cell Cancer Stage II A and B
- The Pancreas as a Site of Metastasis or Second Primary in Patients with Small Bowel Neuroendocrine Tumors
- Effective Cytoreduction Can Be Achieved in Patients with Numerous Neuroendocrine Tumor Liver Metastases
- A Population-based Validation of the Notch Activation in Endothelial Cells by the S. Aureus Toxin HLA Circumvents Transcription of Canonical Downstream Targets
- A 5-year Longitudinal Study of Factors Influencing Surgery as a Career Choice in Medical Students: Analysis of the First Cohort from the Start of Medical School to Matriculation
- Risk Factors for 30-day Readmission Following Adrenalectomy
- Genetic Testing in Breast Cancer Patients: Do Mutations Other than BRCA Make a Difference in Surgical Decision Making?
- Pediatric Trauma Center Verification Improves Clinical Care and Reduces Charges in Children with Blunt Splenic Injury
- The Impact of Patient Demographics vs. Tumor Factors on the Prognosis of Anal Squamous Cell Carcinoma Treated with Standard Chemoradiation Therapy.
- The Equivalence of Short-term Perioperative Outcomes Among Pediatric Patients Undergoing Laparoscopic and Open Ileoanal Pouch Anastomosis
- The Impact of Multiagent Chemoradiation Treatment vs. Radiation With or Without Monoagent Chemotherapy on the Prognosis of Anal Squamous Cell Carcinoma
Innovations
Our Traditions
For nearly 150 years, surgeons have been trained at the University of Iowa. We have been responsible for some of the world’s surgical firsts. Our environment encourages innovative thinking with strong collaboration across many disciplines.
Our Programs
Our aim is to give you the opportunity to chart your course, as a general surgeon or as a specialist. Our rotation schedule and the variety in our case loads, provides you with ample experiences. Our programs are committed to balancing the experiences of fellows and residents to provide each with significant roles in patient care.
Our Technology
Our more than 30 ORs and hundreds of other procedure areas are in heavy demand, year-round. Our department is at the heart of the UI Hospitals and Clinics Center for Procedural Skills and Simulation, providing state-of-the-art systems for training in all facets of surgical procedures.
Our Care
We hold the country’s highest designation for several of our clinical services, a testament to the vision and dedication of our faculty care givers. In some cases, we’ve written the criteria for credentialing programs around the country to deliver effective treatment for complex conditions.
Our Goal
Changing Medicine. Changing Lives. We change medicine each day by asking the difficult “what if” questions. In doing so, we bring better outcomes for hundreds of lives each day. We prepare our residents to be compassionate and innovative healers and discoverers and invite them to join us on this quest to improve the human condition.
How to Apply

We participate in the Electronic Residency Application Service (ERAS).
Carefully follow the ERAS instructions when submitting the required documentation.
Required Documentation
- MyERAS Application
- Medical School Program Evaluation or Dean's Letter
- Transcripts
- Photo
- Three letters of recommendation
- USMLE Step 1 Score (Step 2 Score if completed by your interview date)
- Personal statement
- Curriculum Vitae
All applications must be processed through ERAS, as no paper applications are accepted.
We review the entire application and consider all aspects of the application. Scores and grades are important and are considered as part of the entire application.
American Board of Surgery Certification
Medical specialty certification in the United States is a voluntary process which serves multiple purposes for the trainee and the public.
Certification is:
- one mission of the training program to produce trainees who meet board eligibility criteria;
- distinguishes a physician as someone with a distinct level of expertise;
- provides more opportunities when applying for employment;
- presents resources and tools by the ABMS;
- a commitment to life-long improvement for providing the best patient care; and
- elevates physicians into the ranks of doctors committed to the highest standards of healthcare.
For more information visit the American Board of Surgery.
Our People
Our faculty members bring valuable perspectives from their training around the country. The more than 50 faculty members in our department represent all surgical specialties and bring to their work a dedication to surgical education. As teachers and mentors, our goal is to bring out your best as a surgeon.
Your fellow residents are, just like you, dedicated to rewarding and meaningful careers in the practice of surgery. They come to Iowa from around the world, drawn here by a comprehensive training program, outstanding work environment, and the prospect of practice opportunities and further training afforded by their experiences here.
Our patients are also part of the training equation. They come to University of Iowa Health Care to receive the very best care from experts who are passionate about delivering it in a personable way. As Iowa’s only academic medical center, we see a comprehensive mix of challenging cases and have the privilege to work with many cultures and languages.
One of the best ways to get familiar with a residency program is to hear what our current residents have to say about their experiences.
Our residents would welcome hearing from you directly, via email or through social media.
Our Residency Program Leadership

James De Andrade, MD
Residency Program Director
Nanette Reed, MD
Residency Program Associate Director

Jen Greer, BA
Residency Program Coordinator

Brandee Baker, BAS
Surgical Education Fellowship Coordinator

Cate Unruh, MEd
Surgical Education Coordinator
Current Residents

Annual Intern welcome event with Drs. Ronald and Paula Weigel at the Herbert Hoover Presidential Museum, July 2022.
Alumni Residents
Beyond Your Residency
Our residents have many choices available to them following their residency training.
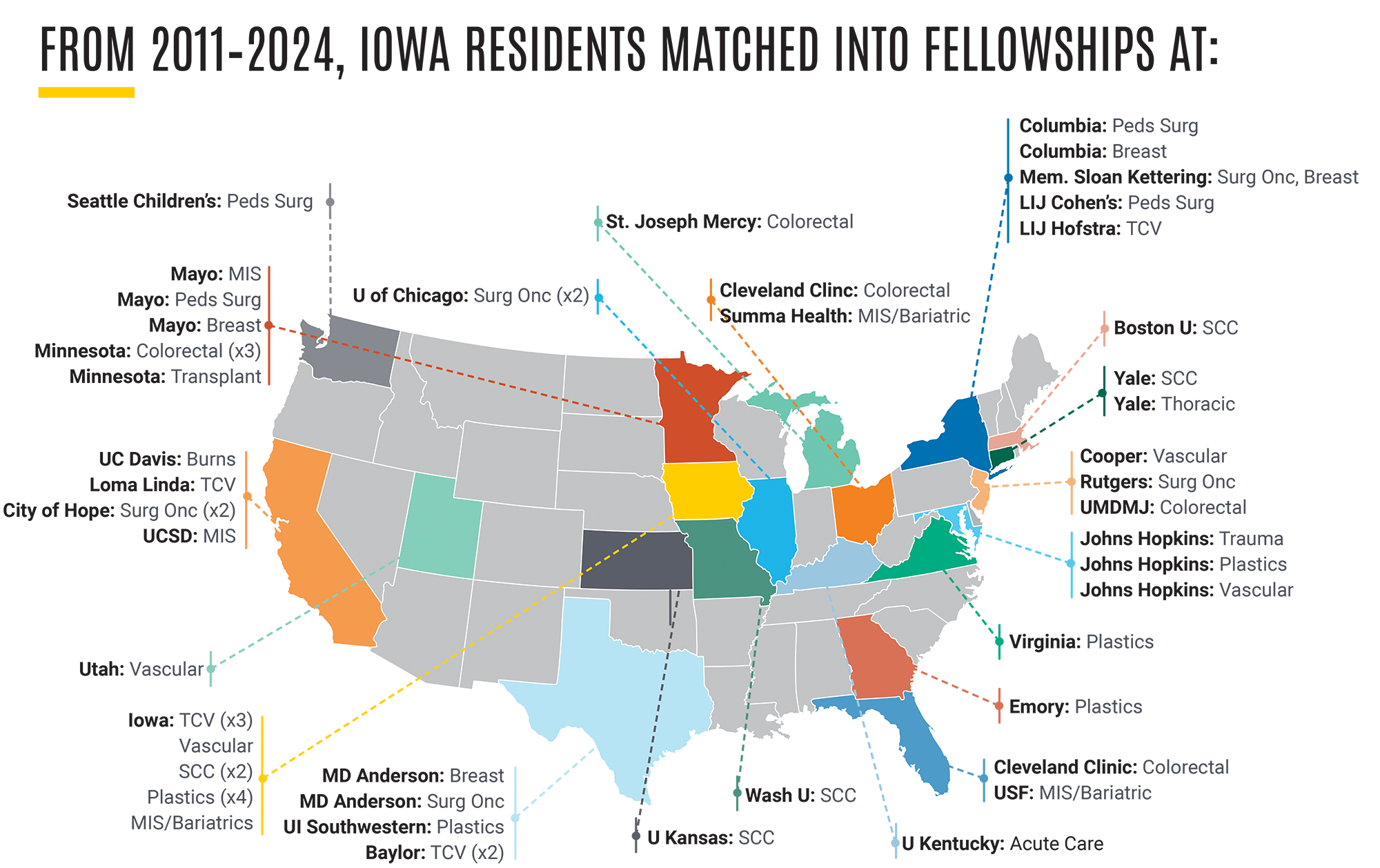
Our department excels in placing residents in subspecialty training in competitive fellowships here and around the country.
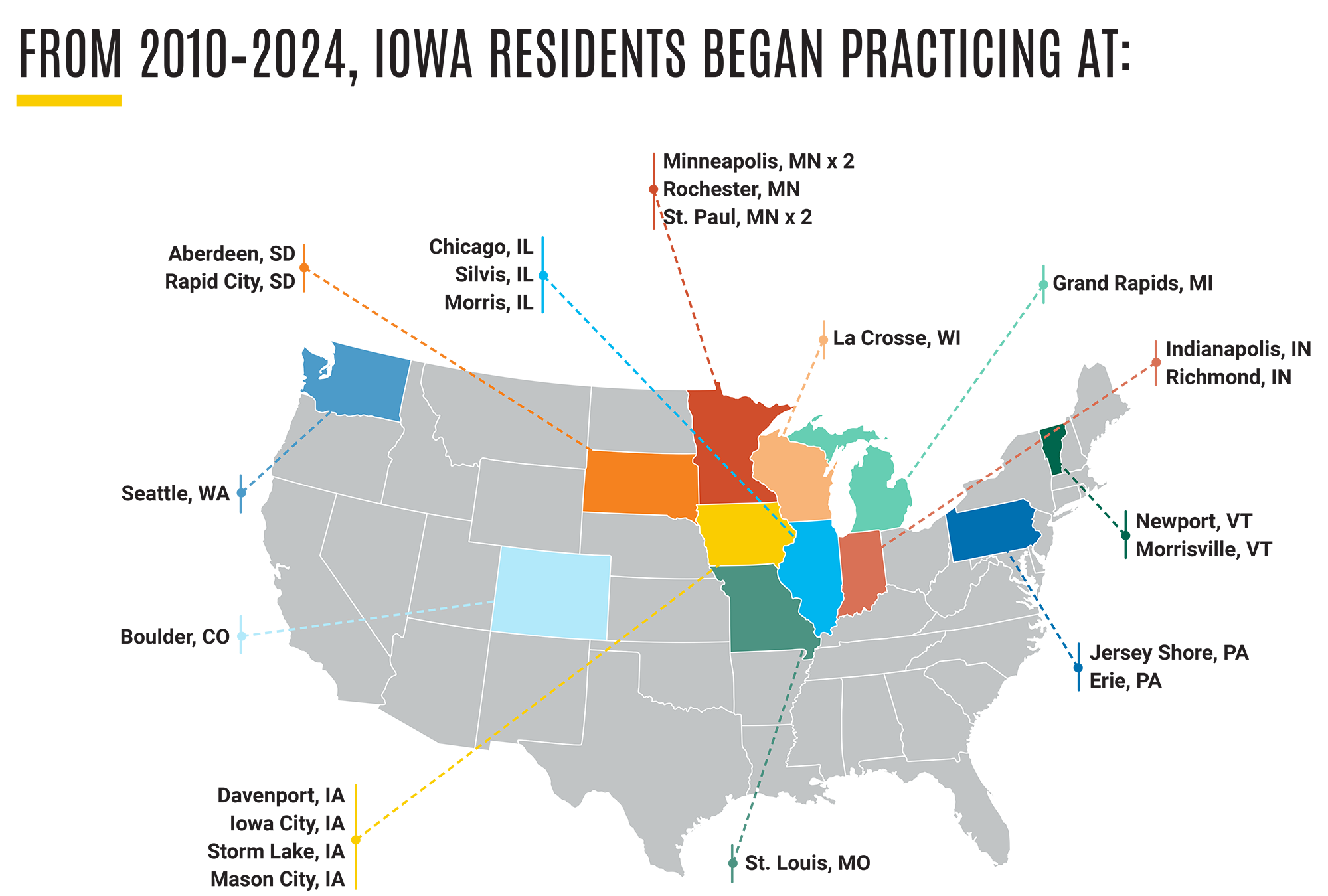
Our residents who elect to go into practice directly find rewarding opportunities available to them, within UI Health Care, in all parts of the country, and in exciting places globally.
Over half of our graduating residents enter fellowship programs and many of them have gone to pursue academic careers. Below is a summary of resident destinations for the past five years.