Vascular Surgery-Integrated Residency
About the Program
 The University of Iowa Hospitals & Clinics is located in Iowa City, Iowa, which is a college town of 70,000 located on both banks of the Iowa River near the intersection of the U.S. Interstate Highways of 80 and 380 in southwestern Iowa. UI Hospitals & Clinics is a tertiary referral base for the State of Iowa and several surrounding states. The Vascular Surgery Section was established in the Department of Surgery in 1987 and became the Vascular Surgery Division in the Department of Surgery in 2001. The Vascular Surgery Fellowship began in 1985 and the Vascular Surgery Residency began in 2013.
The University of Iowa Hospitals & Clinics is located in Iowa City, Iowa, which is a college town of 70,000 located on both banks of the Iowa River near the intersection of the U.S. Interstate Highways of 80 and 380 in southwestern Iowa. UI Hospitals & Clinics is a tertiary referral base for the State of Iowa and several surrounding states. The Vascular Surgery Section was established in the Department of Surgery in 1987 and became the Vascular Surgery Division in the Department of Surgery in 2001. The Vascular Surgery Fellowship began in 1985 and the Vascular Surgery Residency began in 2013.
Rotation Schedule
The following tables are a sample rotation schedule for residents broken down by PGY level. Each academic year is comprised of 13 4-week rotation blocks.
| Block | Specialty |
|---|---|
| 1 | UI Hospitals & Clinics Vascular Surgery |
| 2 | UI Hospitals & Clinics Vascular Surgery |
| 3 | Emergency General Surgery |
| 4 | Transplant |
| 5 | VA General Surgery |
| 6 | Night Float |
| 7 | Plastic Surgery |
| 8 | UI Hospitals & Clinics Vascular Surgery |
| 9 | Trauma |
| 10 | Transplant |
| 11 | Burn Surgery |
| 12 | Plastic Surgery |
| 13 | Trauma |
| Block | Specialty |
|---|---|
| 1 | Catheterization Lab |
| 2 | Catheterization Lab |
| 3 | Surgical Intensive Care Unit |
| 4 | Surgical Intensive Care Unit |
| 5 | Night Float |
| 6 | Pediatric Surgery |
| 7 | Pediatric Surgery |
| 8 | Emergency General Surgery |
| 9 | Colorectal Surgery |
| 10 | Emergency General Surgery |
| 11 | Vascular Lab |
| 12 | VA Vascular Surgery |
| 13 | UI Hospitals & Clinics Vascular Surgery |
| Block | Specialty |
|---|---|
| 1 | Emergency General Surgery |
| 2 | Plastic Surgery |
| 3 | Transplant |
| 4 | Night Float |
| 5 | Cardiothoracic Surgery |
| 6 | Emergency General Surgery |
| 7 | UI Hospitals & Clinics Vascular Surgery |
| 8 | UI Hospitals & Clinics Vascular Surgery |
| 9 | UI Hospitals & Clinics Vascular Surgery |
| 10 | UI Hospitals & Clinics Vascular Surgery |
| 11 | UI Hospitals & Clinics Vascular Surgery |
| 12 | UI Hospitals & Clinics Vascular Surgery |
| 13 | UI Hospitals & Clinics Vascular Surgery |
| Block | Specialty |
|---|---|
| 1 | VA Vascular Surgery |
| 2 | VA Vascular Surgery |
| 3 | VA Vascular Surgery |
| 4 | VA Vascular Surgery |
| 5 | UI Hospitals & Clinics Vascular Surgery |
| 6 | UI Hospitals & Clinics Vascular Surgery |
| 7 | UI Hospitals & Clinics Vascular Surgery |
| 8 | UI Hospitals & Clinics Vascular Surgery |
| 9 | UI Hospitals & Clinics Vascular Surgery |
| 10 | UI Hospitals & Clinics Vascular Surgery |
| 11 | UI Hospitals & Clinics Vascular Surgery |
| 12 | UI Hospitals & Clinics Vascular Surgery |
| 13 | UI Hospitals & Clinics Vascular Surgery |
| Block | Specialty |
|---|---|
| 1 | UI Hospitals & Clinics Vascular Surgery |
| 2 | UI Hospitals & Clinics Vascular Surgery |
| 3 | UI Hospitals & Clinics Vascular Surgery |
| 4 | UI Hospitals & Clinics Vascular Surgery |
| 5 | VA Vascular Surgery |
| 6 | VA Vascular Surgery |
| 7 | VA Vascular Surgery |
| 8 | VA Vascular Surgery |
| 9 | UI Hospitals & Clinics Vascular Surgery |
| 10 | UI Hospitals & Clinics Vascular Surgery |
| 11 | UI Hospitals & Clinics Vascular Surgery |
| 12 | UI Hospitals & Clinics Vascular Surgery |
| 13 | UI Hospitals & Clinics Vascular Surgery |
Rotation Description
UI Hospitals & Clinics Vascular Surgery
Residents rotating on this service will receive training in procedures including: open and endovascular repair of aneurysms, carotid endarterectomy, creation of arterial venous fistulas for hemodialysis, and lower extremity vascular bypass. The mid-level resident is in charge of the outpatient endovascular procedures performed in the cardiac cath lab which include primarily diagnostic and therapeutic angio/venograms as well as vascular access.
VA General Surgery
This is the general surgery consult service for the Iowa City Veterans Affairs hospital, located across the street from the University of Iowa. Similar to the University service, residents develop the skills to efficiently and thoroughly evaluate patients and treat for "bread and butter" issues including appendicitis, cholecystitis, bowel obstruction, hernia, and perforated viscera. Additionally, renal transplants and thoracic procedures are performed at this VA.
VA Vascular Surgery
Residents rotating on this service will receive training in procedures including: open and endovascular repair of aneurysms, carotid endarterectomy, creation of arterial venous fistulas for hemodialysis, and lower extremity vascular bypass.
Vascular Lab
Trainees on this rotation will have dedicated time in the vascular lab. They will work alongside vascular lab technicians in an IAC certified lab in order to gain first-hand experience in duplex ultrasound scanning and other noninvasive vascular lab testing. They will read all of the vascular lab studies done during their rotation allowing them to meet their requirement to sit for their RPVI test.
Vein Clinic
Residents on this rotation will have time dedicated to the evaluation, work-up and treatment of patients with venous diseases. They will receive training in saphenous ablation, phlebectomies, perforator ablation, sclerotherapy and foam sclerotherapy.
Burn Surgery
As the only Burn Treatment Center in Iowa, this service provides exposure to a diverse set of patients of all ages and with all mechanisms of burn and soft tissue injury. In addition to treating patients with chemical, electrical, and thermal energy burns, residents will care for individuals with severe frostbite injuries and necrotizing soft tissue infections. Residents learn management of the acutely injured burn patient, wound care, and skin harvesting and grafting.
Cardiothoracic Surgery
Residents rotating with this service are involved with cardiac surgeries on pediatric and adult patients. Working with thoracic surgeons, they receive training in procedures including esophagectomies, resections of mediastinal masses, and thoracoscopic and open lung resections. They will also gain experience in heart and lung transplantation.
Catheterization Lab
This is one of several rotations during which residents will have the opportunity to develop their endovascular skills. Specifically for this rotation, residents will have their time dedicated to the endovascular suite where they will participate in peripheral interventions and line placement under the direction of the vascular surgery faculty.
Emergency General Surgery
This is the general surgery consult service for the University. Residents rotating on this service develop the skills to efficiently and thoroughly evaluate and treat patients with "bread and butter" surgical issues including appendicitis, cholecystitis, bowel obstruction, hernia, and perforated viscera.
GI Surgery
This service encompasses the breadth of benign and malignant diseases of the small bowel, colon, rectum and anus. Residents rotating on this service learn lower endoscopy and are trained in open, laparoscopic, and robotic approaches to a variety of colorectal conditions. Additionally, this service encompasses the University of Iowa Obesity Surgery, a bariatric Center of Excellence, where residents gain significant experience in gastric bypass surgery, laparoscopic experience performing ventral and inguinal herniorrhaphy, paraesophageal hernia repair and Nissen fundoplication, cholecystectomies via a minimally-invasive approach.
Interventional Radiology
During this rotation, residents will have the opportunity to work with interventional radiologists in the interventional radiology suites covering the breadth of interventions from basics of angiography to complex embolizations.
Night Float
This team is a combination of Trauma and Emergency General Surgery services. Residents are responsible not only for evaluation and treatment of trauma patients and general surgery consults, but they also provide cross-coverage for surgical patients admitted during the day.
Pediatric Surgery
Residents rotating on this service are exposed to elective and emergent surgeries for all ages, from premature neonates to teenagers. The team also manages pediatric trauma patients. It works closely with the Pediatric Gastroenterology team as well as the NICU and PICU. Across all pediatric ages, residents gain varied experience operating in the neck, thorax, and abdomen through both open and laparoscopic approaches. Common neonatal procedures performed include closure of gastroschisis and omphalocele, treatment of tracheoesophageal fistulas, repair of congenital diaphragmatic hernias, and management of necrotizing enterocolitis.
Plastic Surgery
Residents learn a diverse set of procedures such as scar revision, liposuction, post-mastectomy breast reconstruction, component separation for hernia repair, and microvascular free flaps.
Surgical Intensive Care Unit
Rotating in the SICU provides an unparalleled opportunity to care for a diverse set of critically ill patients. Working with critical care specialists trained in surgery, anesthesia, medicine, and pharmacy, residents are part of a multidisciplinary team managing patients with complex needs. Residents learn ventilator management, vascular access, tracheostomy and PEG placement, and neurologic monitoring.
Transplant
This service specializes in liver, pancreas, and kidney transplantations, as well as in hepatobiliary procedures. Residents are trained in the harvesting of organs for transplant, including laparoscopic donor nephrectomies, as well as in the transplantation of these organs. Hepatobiliary procedures performed include those for benign and malignant conditions. Preoperative management of the transplant and hepatobiliary patient is emphasized. Residents will work closely with members of the Transplant Hepatology and Transplant Nephrology Teams.
Trauma
UI Hospitals & Clinics is the only Level 1 Trauma Center in the state, caring for seriously injured patients. Residents on the trauma service learn to rapidly assess and treat these patients, as well as to manage their overall cares once stabilized. The trauma team works closely with other surgical sub-specialties to coordinate and meet patients' treatment needs. All general surgery residents will be ATLS certified. Common procedures performed on this service include: FAST exam, chest tube placement, central line placement, tracheostomies, and trauma laparotomies.
Conference Schedule
Conference Schedule
| Monday | |
|---|---|
| Surgery Resident Education Conference | |
| Vascular Surgery Journal Club | First Monday of Every Month |
| Tuesday | |
| Surgical Audit Conference | |
| VA Vascular Surgery Case Conference | |
| Vein Conference | Every Other Week |
| Surgery Grand Rounds | |
| Wednesday | |
| Surgical Skills Lab | |
| Thursday | |
| UI Hospitals & Clinics Vascular Surgery Case Conference |
Conference Description
Surgery Resident Education Conference
This conference is held on Mondays at 7 a.m. and is for the PGY1s, PGY2s, and PGY3s when on a General Surgery service. The format of this conference utilizes a flipped classroom educational approach, where residents will be assigned weekly modules from SCORE (the General Surgery Resident Curriculum Portal). At the start of the conference residents will complete a short quiz, which will be reviewed by assigned faculty who serve as content experts and who will bring interactive case scenarios to be discussed after the review of the quiz.
Vascular Surgery Journal Club
This conference is held on the first Monday of the month. Four articles are chosen by faculty. The articles are then presented by the vascular fellows and senior residents. This is followed by a discussion with the trainees and staff.
Surgical Audit Conference
This conference is held on Tuesdays at 7 a.m. The content of this conference focuses on cases selected to present and an appropriate literature review in order to improve patient care and reduce complications. Residents selected to present cases, work with faculty members in the development of presentation.
VA Vascular Surgery Case Conference
This is conference is held on Tuesdays at 8 a.m. Midlevel residents and the VA fellow present the cases for the upcoming week. Following a discussion of the relevant clinic indications, the current in-house patients are reviewed.
Vein Conference
This is a bi-weekly conference held on Tuesdays at 3 p.m. During the first half of the conference a resident presents a topic pertinent to venous disease. Following this, interesting or pertinent vein cases are presented for discussion.
Surgery Grand Rounds
This conference is held Tuesdays from September through June on Tuesdays at 4:30 p.m. As surgical science and practice progresses rapidly, a need exists to continuously keep abreast of advances in surgical education, practice, and research. Utilizing visiting experts and local faculty members, development in these areas are formally presented and discussed.
Surgical Skills Lab
Skills lab sessions are held on Wednesdays at 7 a.m. A skills lab curriculum is developed allowing for the residents, based upon level, to learn skills in a controlled environment allowing for verifiable proficiency to be achieved. Sessions are led by department faculty and include formal presentations followed by hands-on practice.
UI Hospitals & Clinics Vascular Surgery Conference
This conference is held on Thursdays at 4 p.m. The conference is led by the fellows who present complex vascular cases. This is followed by discussion that is aimed to engage medical students, junior and senior residents as well as the fellows and staff.
Research Opportunities
Research is an important part of the daily activities of all academic surgeons. The continuing commitment to productive scholarship, embodied by research, as much as a commitment to communicative scholarship, exemplified by teaching, distinguishes the academic surgeon from his/her colleague in nonacademic practice.
The obvious benefit of research to our patients and to the community is improved care. Less obvious, but equally important, benefits are the atmosphere of open and rigorous inquiry, the constant questioning and the intellectual stimulation which the research programs provide to their participants - faculty, residents, and medical students.
There are numerous opportunities to become involved in basic science and/or clinical research, which leads to the development of many projects that are presented at regional and national meetings. Please use the following link for information concerning research within the Department of Surgery.
How to Apply
Our program participates in the Electronic Residency Application Service (ERAS). Your ERAS Application will contain the following documentation, which is required when applying for our program:
- MyERAS Application
- Medical School Program Evaluation or Dean's Letter
- Transcripts
- Photo
- Three letters of recommendation
- USMLE Step 1 Score (Step 2 Score if completed by your interview date)
- Personal statement
- Curriculum Vitae
All applications must be processed through ERAS, as no paper applications are accepted.
American Board of Surgery Certification
Medical specialty certification in the United States is a voluntary process which serves multiple purposes for the trainee and the public.
Certification is:
- one mission of the training program to produce trainees who meet board eligibility criteria;
- distinguishes a physician as someone with a distinct level of expertise;
- provides more opportunities when applying for employment;
- presents resources and tools by the ABMS;
- a commitment to life-long improvement for providing the best patient care; and
- elevates physicians into the ranks of doctors committed to the highest standards of healthcare.
For more information visit the American Board of Surgery.
Our People
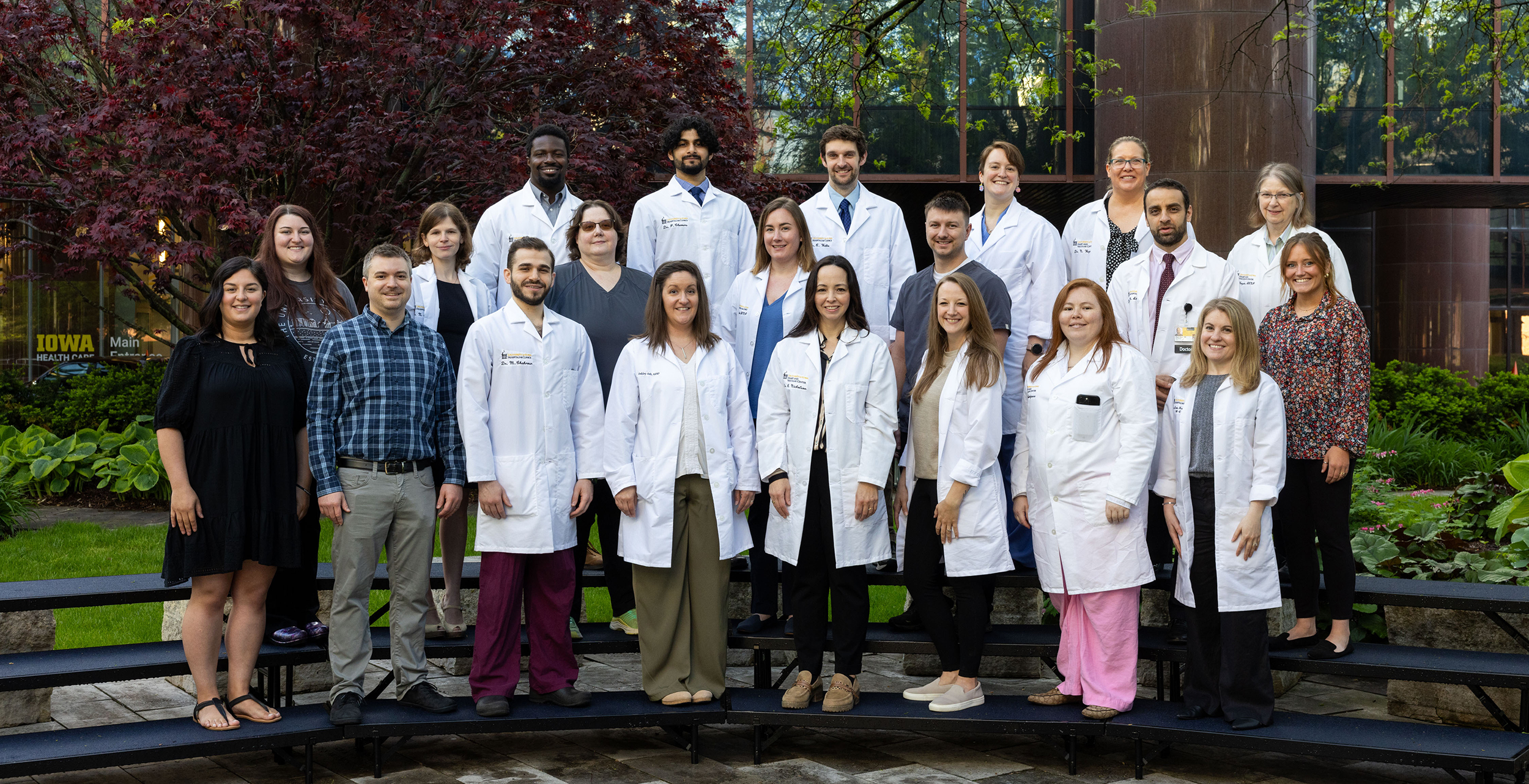
Faculty Members
The Division of Vascular Surgery has faculty members who hail from other top institutions from around the country, each bringing with them a unique surgical perspective that will add depth to your skill-set.
Rachael Nicholson, MD
Division of Vascular Surgery – Interim Director
Program Director, Vascular Surgery Residency
Program Director, Vascular Surgery Fellowship
Medical Director, Peripheral Vascular Laboratory
Clinical Associate Professor, Surgery
Maen Aboul Hosn, MD
Interim Chief of Surgery, VAMC
Associate Program Director, Vascular Surgery Residency
Associate Program Director, Vascular Surgery Fellowship
Clinical Assistant Professor, Surgery, Division of Vascular Surgery
Chief of Vascular Surgery, VAMC

Adeola Odugbesi, MD
Clinical Assistant Professor, Surgery, Division of Vascular Surgery
Natalie Weger, DO
Clinical Assistant Professor, Surgery, Division of Vascular Surgery
Co-Clerkship Director, Surgery Core Clerkship
Current Residents
Academic Year July 1, 2024 – June 30, 2025
First Year Resident

Salim Habib, MD
Medical School: American University of Beirut Faculty of Medicine
Second Year Resident
Ryan Watts, DO
Medical School: Campbell University - School of Osteopathic Medicine
Third Year Resident
Phani Chevuru, MD
Medical School: University of Iowa RJ & L Carver College of Medicine
Third Year Resident
Mohamad Chahrour, MD
Medical School: American University of Beirut Faculty of Medicine
Fourth Year Resident
Victor Hatcher, MD
Medical School: University of Iowa RJ & L Carver College of Medicine
Current Fellows
We currently accept one Fellow every other year.
2024-2025 Vascular Surgery Roster
Megan Parrott, MD
Medical School: University of South Carolina School of Medicine
Alumni Fellows
2021-2023
John E. Muhonen, DO
2019-2021
Sarah Burger, MD
Medical school: Medical College of Wisconsin
Residency: University of Iowa Hospitals & Clinics
2016-2018
Samantha Alsop, MD, MPH
Medical school: University of Kansas School of Medicine
Residency: University of Kansas
Private practice: Kansas City, Mo.
2015-2016
James Foster, III, MD
Medical school: University of Missouri-KC School of Medicine
Residency: University of Missouri-KC
Private practice: Kansas City, Kan.
Contact Us
Medical Center at the University Campus
Department of Surgery - Vascular Surgery Residency Program
200 Hawkins Drive
Iowa City, IA 52242
Ferial Ebrahim-High,BA,BHSc(Hons)
1-319-356-8474
Email: ferial-ebrahim-high@uiowa.edu
Alumni Residents
2024 Graduate
Nicole Gensicke, MD
Private Practice in Cedar Rapids, IA
2023 Graduate
Crystal Rodriguez, MD
University of Iowa Hospitals and Clinics
2022 Graduate
Jeanette Man, MD
Private Practice in Green Bay,WI
2021 Graduate
Adeola T. Odugbesi, MD
University of Iowa Hospitals and Clinics
2020 Graduate
Anna Marjan, MD
Private Practice: Minneapolis, MN
2019 Graduate
Justin Walpole, MD
Private Practice: Grand Junction, CO
2018 Graduate
Ryan Deets, MD
Private Practice: Burlington, IA
2017 Graduate
Maen Aboul-Hosn, MD
University of Iowa Hospitals and Clinics