About the Program
 The seven-year neurosurgical residency program at the University of Iowa is designed specifically to prepare residents for a career as senior surgeon-scientists, and future leaders in the field of academic neurosurgery. It is the intent of this seven-year training program to develop world class neurosurgeons.
The seven-year neurosurgical residency program at the University of Iowa is designed specifically to prepare residents for a career as senior surgeon-scientists, and future leaders in the field of academic neurosurgery. It is the intent of this seven-year training program to develop world class neurosurgeons.
Residents completing the program will be eligible for certification by the American Board of Neurological Surgery (ABNS) with a goal of a 100 % pass rate on both the qualifying and the certifying examinations. Categorical residents are required to pass the written examination for primary certification, prior to becoming chief resident. Visit the American Board of Neurosurgical Surgery for specifics on board certification requirements.
Clinical competencies
To attain these goals, the program requires residents to develop the following competencies:
- A solid foundation of basic and clinical knowledge of neurosurgery.
- The ability to provide compassionate and effective care to all patients.
- The ability to perform general neurosurgical procedures safely and effectively.
- The exercise of clinical judgment to critically select the appropriate course of action in the management of patients.
- The capacity to communicate effectively with all healthcare personnel and with patients.
- Knowledge about established and emerging biomedical, clinical and cognitive sciences, and the application of this knowledge to neurosurgical patient care.
- Ability to analyze practice experience and perform practice-based improvement activities using a systematic methodology.
- Apply knowledge of study designs and statistical methodology to the appraisal of clinical studies and information regarding diagnostic and therapeutic effectiveness.
- A demonstrated commitment to carrying out professional and administrative duties, adherence to ethical principles and sensitivity of diverse patient populations, required in the surgical profession.
- The constant pursuit of improvement in patient care practices by systematic evaluation of current practices in relation to outcomes and to new scientific knowledge.
- An awareness of and responsiveness to the underpinnings of the health care system, and the dilemmas of practicing healthcare that is of optimal value and cost effective.
Residents are expected to develop these elements of clinical competence by doing the following:
- Assimilating the teaching provided by the faculty
- Maintaining an active reading plan for neurosurgical sciences
- Practicing their clinical/surgical skills
- Attending the educational activities offered by the residency program
Assessments
During the seven years of intensive training, each of the above elements of clinical competence is periodically assessed by direct faculty supervision and by senior resident colleagues with subsequent review by the program director. Re-appointment and promotion to the subsequent PGY year requires a satisfactory progression in the development of these elements of clinical competence.
The educational program of the residency is designed to meet specific goals and objectives at each level of training as outlined in the following table. The program is designed in accordance with the ACGME core competencies. RRC requirements can be found on the ACGME Neurological Surgery site.
PGY by Year

PGY-1
During the PGY 1 year the resident spends six months on the neurosurgical service taking care of patients on the neurosurgical floor and getting early exposure to the operating room Residents learn the following in their first year:
- Preoperative medical work-up for neurosurgical patients
- Postoperative care & critical care management of the neurosurgical patient
- Complex socioeconomic factors related to disposition
In addition to inpatient care, the resident is expected to become comfortable in operating room. Under the supervision of faculty and senior residents, the PGY-1 resident will be expected to become proficient with the following:
- Positioning & Equipment Setup
- Standard opening & closing of cranial & spinal procedures
- Basic operative technique
- Ventriculostomy Placement
- Intracranial Pressure Monitor Placement
- Lumbar Drain Placement
PGY 1 residents take "buddy call" with the PGY 2 and 3 residents and, in a graduated fashion, learn the structure, organization, and work-up necessary for being the independent on-call resident.
Off-service rotations
The remainder of the PGY 1 year is spent on off service rotations providing exposure to services that work closely with the neurosurgical service, cultivating a deeper understanding and appreciation for the overall care of the patients that we manage.
These include:
- Trauma surgery
- Stroke neurology
- Neuroendovascular Surgery (working in the angiography suite with Neurosurgery/Neurology/Radiology)
- Neuro-otology (exposure to lateral skull base approaches)
- Neuro-ophthalmology
- Surgical-Neurological ICU
PGY-2 and PGY-3 (18 months on inpatient service)
During the PGY 2 and 3 years, residents are fully integrated into the neurosurgical service and assume the role of “junior resident,” including primary call responsibility, graduated autonomy in the operating room, and management of the inpatient service.
Junior resident call is a 24-hour in-house call that, on average, is taken every 4 days. During the on-call period, the resident is responsible for every aspect of the neurosurgical service, allowing the resident to develop extensive knowledge and experience caring for critically ill patients on our service
Resident responsibilities
This includes the following responsibilities:
- Knowing the neurologic exam and plan for every patient on the neurosurgical service
- Reviewing the imaging studies acquired on such patients
- Evaluating patients postoperatively
- Seeing new consults in the emergency room
Promptly to any questions/pages regarding any patient on the neurosurgery service
During this time, each resident is also assigned to a primary service, with each rotation consisting of a 6-month block.
These include:
- Intensive Care Unit (ICU) patients
- Pediatric Neurosurgical patients
- Neurosurgery consultation patients
In the operating room, the junior resident continues to advance their operative skills, gaining progressive autonomy in increasingly complex procedures under the supervision of the attending neurosurgeon. This includes exposure to vascular neurosurgery, neuro-oncology, epilepsy surgery, complex spine surgery, and functional neurosurgery, peripheral nerve surgery, and endovascular neurosurgery.
PGY-3 – 6 months on Continuity of Care (CoC) rotation
During this 6-month rotation the resident begins to transition into a more senior resident role with an independent block with two faculty, Hiroyuki Oya, MD, PhD, and Satoshi Yamaguchi, MD, PhD.
The resident will be paired with these faculty in a “mentorship model” in which they follow their patients from clinic, to the operating room, and to follow-up.
During this time, the resident spends two days a week in the clinic with these faculty evaluating patients and then is able to follow these patients through their entire interaction with the neurosurgical service.
This time allows the resident to gain further experience in the following areas.
- Outpatient evaluation of neurosurgical disease
- Patient History & Physical
- Imaging assessment
- Formulating a surgical plan & discuss management strategies
- Ongoing evaluation & management of neurosurgical patients
- Review procedures and consent information with patients
- Perform operate procedures with faculty oversight
- Round on and manage postoperative patients
- Patient follow-up in clinic after discharge
This rotation has been invaluable to the education of the neurosurgical resident in allowing them to gain a greater appreciation of the entire scope of patient care as they move toward independent practice, from outpatient evaluation, surgical intervention, and follow-up care. Focused mentorship during this time also allows the resident to gain autonomy in patient management as well as in the operating room, allowing significant advancement in operative skill.
PGY-4 and PGY-5 – 2 years of research time
After completion of the junior resident years, the transition to senior residency begins with two years of dedicated research time.
During the initial three years, it is expected that the resident has explored research opportunities and begun working with neurosurgical faculty and colleagues in both the clinical and basic science realms to establish a collaborative research plan.
The goal during this two-year period is to allow the resident dedicated time to be immersed in rigorous scientific research and acquire the skills necessary for a lifelong career as an academic surgeon scientist. Time should be spent executing experiments, analyzing data, and preparing manuscripts for publication.
Clinical responsibilities
Clinical obligations during this time are limited, with the resident covering “chief call” on average 1 of 4 weekends. This involves rounding with the team that weekend and taking home call while supervising the in-house junior resident on call.
All operative procedures during this call period are performed by the resident on “chief call” in conjunction with the attending on call.
PGY-6 - Chief Year
The chief residency year is divided into two six-month blocks during which the chief resident is assigned half of the neurosurgical service based on faculty member. The chief acts as the primary physician responsible for managing all aspects of neurosurgical patient care.
Responsibilities of the chief resident include:
- Rounding on all patients
- Formulating care plans, even for the most complex neurosurgical patients
- Formulating operative plans
- Overseeing the care provided by junior residents
- Providing operative coverage for elective and emergent cases daily
- Alternating call every other day to direct care of new consults
Upon completion of this year under the supervision of the neurosurgical faculty, the chief resident should be prepared to practice and operate independently as they transition independent practice.
PGY-7 – Transition to Practice
During the PGY-7 year, the resident spends six months at the University of Iowa where they will see patients in their own clinic and to formulate clinical and operative plans independently. These patients will be staffed with a supervising faculty member who ultimately is responsible for the case, however it is the expectation that the PGY-7 resident acts as the treating physician.
Buddy call
In addition to the elective outpatient service, the resident also will take "buddy" faculty call to further the transition to practice experience, allowing for independent decision making regarding operative management. Moreover, the PGY 7 resident is available to operate on any of the elective patients on the operative schedule to allow the trainee to further hone their operative skills in an independent, but mentored environment.
Off-site rotation
The other six months of the PGY-7 year is designed to allow the resident additional training in their field of choice. This is frequently done off site at another institution, however if desired the resident may also stay at the University of Iowa and work with any of the faculty in a one-on-one fashion to continue to develop skills of interest.
These experiences are typically arranged independently by the resident prior to their chief year with the guidance of faculty. During this period, the resident is provided with a living expense stipend in addition to their current salary and benefits to offset the cost, allowing the pursuit of additional training in their subspecialty area of focus.
Overall, this has been an invaluable experience during this final year, allowing for significant professional and personal growth.
PGY-7 Elective Opportunities
During the PGY-7 year, residents can spend six months at a location of their choice getting additional training in an area of interest. This may be done off-site or at the University of Iowa and is setup independently by each resident with the guidance of faculty.
Recent locations
Some sites visited by residents in the past include:
- Melbourne, Australia (Pediatrics)
- Sydney, Australia (Tumor/Minimally Invasive)
- England (DBS)
- Northwestern (Spine)
- Rush (Spine)
- Japan
- Africa (Mission work)
- Grenoble, France (sEEG)
- Netherlands
Research Opportunities
 Regardless of your research interest, there is a mentor to be found at University of Iowa Health Care. The environment is collaborative, and whether you want to work inside or outside the Department of Neurosurgery, everyone here is open to receiving a neurosurgery resident with an interest in their area of expertise.
Regardless of your research interest, there is a mentor to be found at University of Iowa Health Care. The environment is collaborative, and whether you want to work inside or outside the Department of Neurosurgery, everyone here is open to receiving a neurosurgery resident with an interest in their area of expertise.
Presenting research
Our weekly Saturday conference gives an opportunity for you to present your research interests and progress to Dr. Howard for feedback, research mentoring, and career advice with the rest of your resident team. This is an opportunity to hone your research skills and receive guidance by Dr. Howard's expertise in collaborative research team building to help you become an academic surgeon scientist at the highest level.
Visiting professors
If there is an expert in your chosen field, it is easy to work with Dr. Howard to have that person come as a visiting professor to give a talk and give you a chance to form a collaboration together. For residents interested, there is also plenty of support during the research grant-writing process.
Resident Benefits
Learn about the benefits provided by the University of Iowa Graduate Medical Education.
Conference Schedule

Mondays
Morbidity/Mortality Conference, Journal club (“Monday Talk”) - 5:00 p.m.
The department meets weekly to discuss Morbidities and Mortalities on the service. Discussion is facilitated to make this a learning experience for residents and faculty alike. Frequently, as time allows, residents can present on a topic of interest that has arisen on service. This is done through a brief presentation of the literature related to the topic and a summary of major points for discussion. The goal of this conference is to foster ongoing learning and improvement of patient care on the Neurosurgical service.
Tuesdays
Neuropathology/Tumor Board - 7:00 a.m.
This weekly conference is attended by neurosurgery faculty and residents, neuroradiology, medical and radiation oncology, as well as neuropathology. Conference alternates between a neuropathology-based teaching conference and tumor board.
The neuropathology conference focuses on the presentation of the histology and immunohistochemical stains used in deriving neurosurgical diagnoses. This is done in an oral board style format with high yield topics discussed in a way to prepare for the neurosurgical boards.
The tumor board conference is a format for presentation of complex tumor pathology with discussion of the radiology and pathology as well as a discussion of the medical and surgical treatment plans for the patient.
Residents are routinely given the opportunity to discuss their interpretation of the imaging and clinical course and devise a management plan can then be discussed in a multidisciplinary fashion and as such gives the resident ample educational opportunity to discuss complex case management.
Wednesdays
Rotating Vascular, Spine, Pediatric, and General Case Conference – 5:00 p.m.
This is a rotating case series once a month held every Wednesday at 5 PM. Depending on the topic a neurosurgical board style presentation of cases including clinical presentation, neurologic exam and imaging studies are presented and each resident is given the opportunity to interpret and diagnose the clinical picture. Residents then offer operative management as appropriate and discuss surgical approaches as well as potential risks and management of complications that may occur. This is done with the neurosurgical faculty present and guiding the discussion and represents a fantastic learning opportunity for residents at all levels of training.
Stroke Conference – 4:00 p.m.
This is an optional conference for residents interested in vascular disease, in the neuro-endovascular management of ischemic disease. Each week cases are discussed from the previous week, including interpretation of imaging as well as intervention taken and patient outcome.
Thursdays
Vascular Conference – 4:00 p.m.
This weekly vascular conference focusses on the endovascular diagnosis and treatment of intracranial and spinal vascular anomalies. This includes, but is not limited to, aneurysms, arteriovenous malformations, and arteriovenous fistulas. Cases from the previous week are discussed and treatment plans are formulated with a multidisciplinary group from neurosurgery, neuroradiology, and neurology.
Fridays
Invited Guest Lecture/Research Conference – 5:00 p.m.
This conference represents our invited guest lecture series. This is either an internal faculty member at the University of Iowa or a visiting professor from an outside institution presenting on their research. This is a wonderful opportunity for residents to invite experts in their fields of interest to present their work and provides an opportunity to foster research collaborations.
In weeks that e no uninvited guest lecture is scheduled, residents are given the opportunity to present an update on their research progress in front of the faculty, who provide constructive feedback and guidance as the resident advances towards their research goals.
Saturdays
Saturday Conference – 8:30 a.m.
Saturday conference is an opportunity for Dr. Howard to meet with all the residents. The major goal of conference is for residents to present their research progress and to have the one-on-one opportunity with Dr. Howard for career counseling with the goal of becoming a successful academic surgeon scientist. When Dr. Howard is out of town, there is opportunity to review anatomy or various other topics with Dr. Greenlee or Dr. Brian Dlouhy.
University of Iowa Human Skull Base Lab
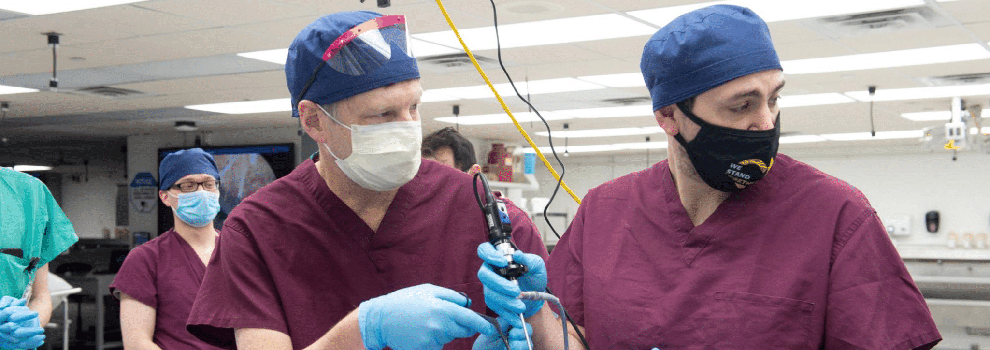
The University of Iowa recently started a cadaver lab with support from industry partners equipped with surgical microscopes, endoscopy, and all the necessary surgical instruments to familiarize residents with common skull base approaches and appreciation of neuroanatomical structures and relationships.
These have included orbitozygomatic, far lateral, interhemispheric, supracerebellar infratentorial, transpetrosal, and expanded endoscopic endonasal approaches in conjunction with our ENT colleagues. Additionally, the University of Iowa has recently begun construction on new wet lab space in the Centers for Procedural Skills and Simulation that will be outfitted with 16 stations with microscopes, drills, and suctions that will be available 24/7 to residents.
Learn more about Center for Procedural Skills and Simulation (CPSS)
Life Outside the Hospital
Iowa City is a college town that provides the ease of living in a small town with the amenities of a big city.
To learn more about housing, schools, transportation and things to do, visit our page about Iowa City.
Clinical Facilities

University of Iowa Health Care is located on the health sciences campus of the University of Iowa. UI Health Care consists of University of Iowa Hospitals & Clinics, University of Iowa Stead Family Children’s Hospital, and the Roy J. and Lucille A. Carver College of Medicine.
UI Health Care is an integral part of the University of Iowa and has a longstanding tradition of excellence in patient care, education, and research. It has long been recognized as one of the leading health care centers in the world.
 University of Iowa Hospitals & Clinics
University of Iowa Hospitals & Clinics
University of Iowa Hospitals & Clinics is a large and well-supported teaching hospital. It provides tertiary level services for the entire state and region, while at the same time creating an environment for health education programs at all levels, and in all specialties.
University of Iowa Hospitals & Clinics clinical services are organized through 22 departments. These include the following:
- Anesthesiology
- Dentistry
- Dermatology
- Emergency Medicine
- Family Medicine
- Internal Medicine
- Neurology
- Neurosurgery
- Obstetrics and Gynecology
- Ophthalmology and Visual Sciences
- Orthopedics and Rehabilitation
- Otolaryngology
- Pathology
- Pediatrics
- Pharmacy
- Psychiatry
- Radiation Oncology
- Radiology
- Rehabilitation Therapies
- Respiratory Care
- Surgery
- Urology
Each clinical service offers residency and fellowship programs as applicable, which are directed by faculty members from the Carver College of Medicine and the College of Dentistry.
Residents who train at UI Hospitals & Clinics experience a commitment to clinical excellence, including quality care delivered in a wide range of services, the most up-to-date medical technology, a medical staff comprised of senior physicians who have national reputations in their fields, excellent nursing and professional staff member with rigorous requirements for quality, and highly respected clinical and basic science research programs.
University of Iowa Stead Family Children's Hospital
University of Iowa Stead Family Children's Hospital is an integral part of UI Health Care. The UI Hospitals & Clinics Pediatric Neurosurgery service provides the only pediatric neurosurgical care in Iowa and draws patients from areas throughout the Midwest.
For particularly complex procedures, UI Hospitals & Clinics Pediatric Neurosurgery attracts patients from across the United States, as well as international patients. The Pediatric Neurosurgery service performs approximately 250 procedures annually, treating patients with hydrocephalus, cranio-vertebral junction abnormalities, plagiocephaly, tumors (both cranial and spinal), and spinal dysraphisms.
Carver College of Medicine
University of Iowa Roy J. and Lucille A. Carver College of Medicine contributes significantly to the strength of University of Iowa Health Care. With a large full-time faculty, the college carries out its functions of education, research, and service. Talented faculty bring fresh ideas, new techniques, and enthusiasm to the teaching of medical students, residents, fellows, and graduate students in various training programs.
The College of Medicine's teaching and basic science facilities are located adjacent to University Hospitals & Clinics, allowing scientists from both basic science and clinical departments to easily pursue interdisc
iplinary research and education.
The faculty, students, resources, and funding at the Carver College of Medicine form the cornerstone of a first-class institution committed to the missions of the patient care, education, and research.
Neurosurgery Sub-Internship
 The Department of Neurologic Surgery at the University of Iowa encourages medical students from the University of Iowa, as well as students from other medical schools, to experience four-weeks immersed in the Iowa neurosurgical service.
The Department of Neurologic Surgery at the University of Iowa encourages medical students from the University of Iowa, as well as students from other medical schools, to experience four-weeks immersed in the Iowa neurosurgical service.
Students are usually senior medical students interested in pursuing a career in neurosurgery with a desire to get more hands-on experience and see how the residency program works.
Sub-Intern activities
The Sub-intern will spend time on the adult and pediatric services rounding with the residents, scrubbing into the operating room cases, and working up patients with the on-call residents. Students will also have an opportunity to present to the department on a topic of their choice, typically a research topic they have spent time on.
Contact information
For additional information or to apply, please contact:
Kathy Escher
319-356-2771
Policies and Procedures
Please review the following policies and procedures from the Department of Neurosurgery.