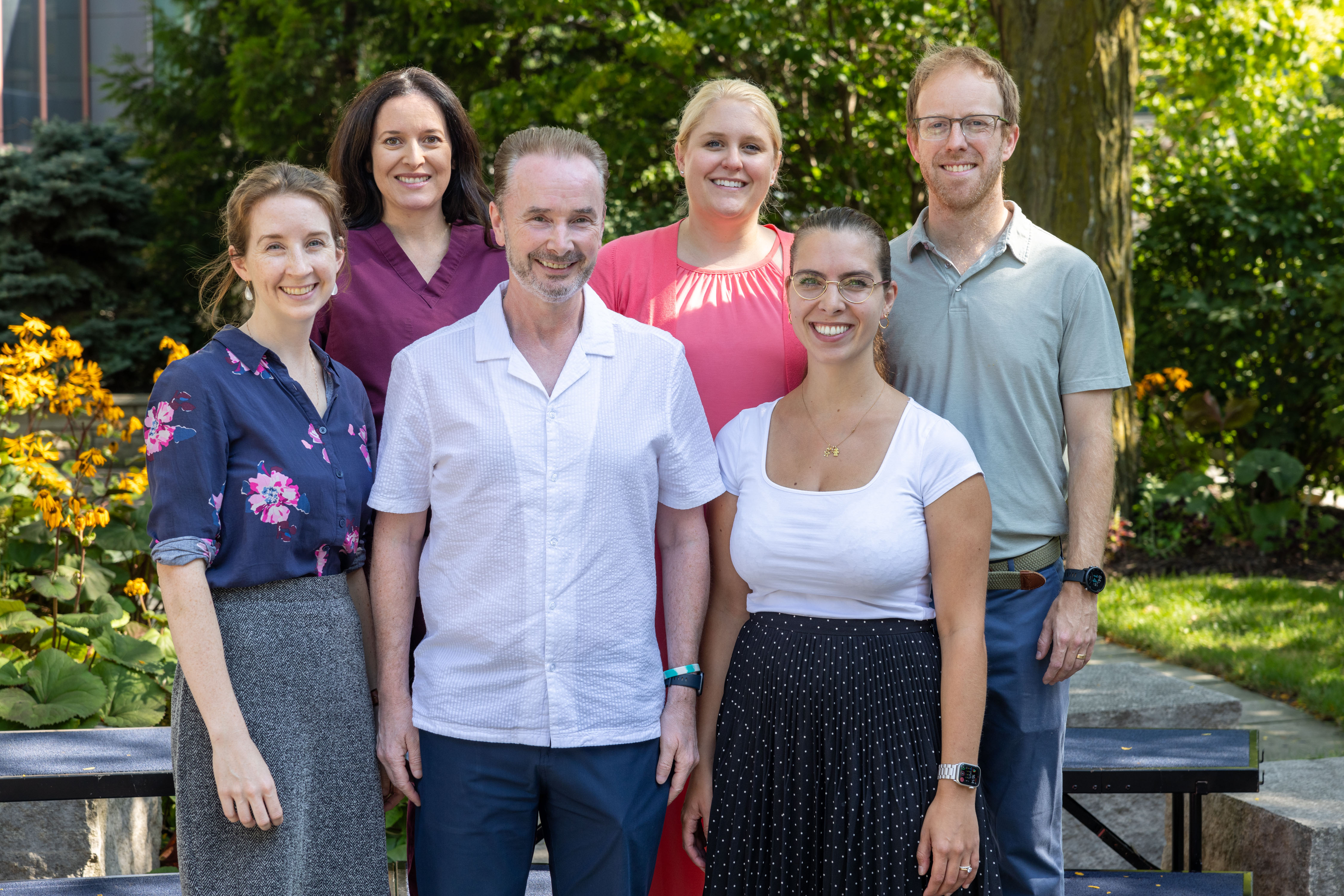
Rachael Hyland, MD
Clinical Assistant Professor
MD, University of Iowa Carver College of Medicine
BA, Washington University, St. Louis, Missouri
Dr. Hyland attended medical school at the University of Iowa Carver College of Medicine and completed her residency in Pediatrics and fellowship in Neonatal-Perinatal Medicine at Washington University in St. Louis. She then returned to Iowa to start her Neonatal Hemodynamics Fellowship in July 2022. Her research interests include the hemodynamic consequences of intrauterine growth restriction, particularly within the extremely premature neonatal population, and the hemodynamics of extra corporeal life support (ECLS/ECMO).
_______________________________________________________________________________________________________________________________________________________________________________________

Patrick McNamara, MB, BCh
Neonatology Division Director; Professor
MB, BCh, BAO, Queens University Belfast, Belfast, Northern Ireland
MRCPCH, Royal College of Physicians and Surgeons of Edinburgh, Edinburgh, United Kingdom
MSc, University of London, London
Through McNamara’s leadership, Iowa’s division of neonatology has become an internationally recognized leader in Neonatal Hemodynamics. In addition to his role as Founder and Chair of the Pan-American Hemodynamics Collaborative, he is the Chair of the Pediatric Academic Society Neonatal Hemodynamics Club and codirector of the Neonatal Hemodynamics Research Center. His clinical and research interests include myocardial performance in the setting of a hemodynamically significant ductus arteriosus, pulmonary hypertension and Targeted Neonatal Echocardiography.
________________________________________________________________________________________________________________________________________________________________________________________

Adrianne Rahde Bischoff, MD
Clinical Assistant Professor
MD, Universidade Federal to Rio Grande do Sul, Porto Alegre, Brazil
Adrianne graduated from medical school at the Federal University of Rio Grande do Sul in her hometown in South Brazil and completed a Pediatrics Residency at the Hospital de Clinicas de Porto Alegre. She pursued her Neonatal-Perinatal training at the University of Toronto and the Hospital for Sick Children where she grew a special interest in the field of Neonatal Hemodynamics and Targeted Neonatal Echocardiography. Adrianne was the first graduate of the Neonatal Hemodynamics Fellowship Program at the University of Iowa. Her research interests include cardiovascular physiology, patent ductus arteriosus definitive closure, and the use of cardiac MRI.
_________________________________________________________________________________________________________________________________________________________________________________________

Danielle R. Rios, MD, MS
Clinical Professor
MD, University of Arizona, College of Medicine, Tucson, Arizona
MS, Clinical Investigation, Baylor College of Medicine, Houston
BS, Child Development, Arizona State University, Tempe, Arizona
Danielle Rios is a Clinical Professor of Pediatrics in the Division of Neonatology at the University of Iowa. She completed residency and neonatology fellowship at Baylor College of Medicine and Texas Children's Hospital where she also completed a Clinical Pharmacology Fellowship. Additionally, she completed a fellowship in Targeted Neonatal Echocardiography at the University of Toronto and Hospital for Sick Children. Her areas of academic focus are the improvement of outcomes in extremely low birth weight infants through predictive analytics and the hemodynamics of neonates born prematurely.
_______________________________________________________________________________________________________________________________________________________________________________________

Amy Stanford, MD
Clinical Assistant Professor
MD, University of Iowa, Roy J. and Lucille A. Carver College of Medicine, Iowa City, Iowa
BS, Biology, Iowa State University, Ames, Iowa
Amy Stanford is an Assistant Clinical Professor of Pediatrics in the Division of Neonatology at the University of Iowa. She completed residency, neonatology fellowship, and neonatal hemodynamic fellowship at University of Iowa. She is establishing our multidisciplinary outpatient Hemodynamic Follow Up Clinic. Her areas of academic focus are chronic pulmonary hypertension and long-term cardiovascular outcomes of prematurity.
_____________________________________________________________________________________________________________________________________________________________________________________

John (Jack) Wren, Jr., MD, PhD
Clinical Assistant Professor
MD, PhD, Wake Forest School of Medicine
BA, Washington University, St. Louis, Missouri
Dr. Wren received his MD, PhD from Wake Forest School of Medicine and completed his residency in Pediatrics at St. Louis Children's Hospital. He went on to Washington University in St. Louis where he completed the Neonatal-Perinatal Medicine Fellowship. He came to the University of Iowa in 2023 for his Neonatal Hemodynamics Fellowship and joined as faculty in July 2024. His research interests include investigating the the role of inflammatory mediators in the pathogenesis of a hemodynamically significant PDA as well as the implementation of hemodynamics-directed care for infants with CDH.
________________________________________________________________________________________________________________________________________________________________________________________